Ovarian Neoplasm
Duration 16:23
Teaching Script: Ovarian Neoplasm
Clinical Case Applicability:
Adnexal Mass, Complications of Metastatic Disease
Learning Objectives:
1) Understand the different cell types involved in ovarian neoplasms
2) Review use of biochemical markers in identifying ovarian neoplasms (CA125 and larger sequence used)
3) Review genetic predispositions to ovarian neoplasm (briefly BRCA and Lynch syndrome)
Clinical Presentation:
Pregnancy with ovarian mass; Perimenopausal with gastrointestinal symptoms and adnexal mass
Considering anatomy and histology of the ovary, what cell types may evolve into ovarian neoplasms?
• Ovarian Anatomy
o Premenopausal ovaries are about 3x2x2 cm in size; suspended between the ovarian ligament medially and the
infundipulopelvic ligament laterally and superiorly.
o Outer cortex: ova and follicles; Inner medulla: fibromuscular layer of blood vessels and connective tissue
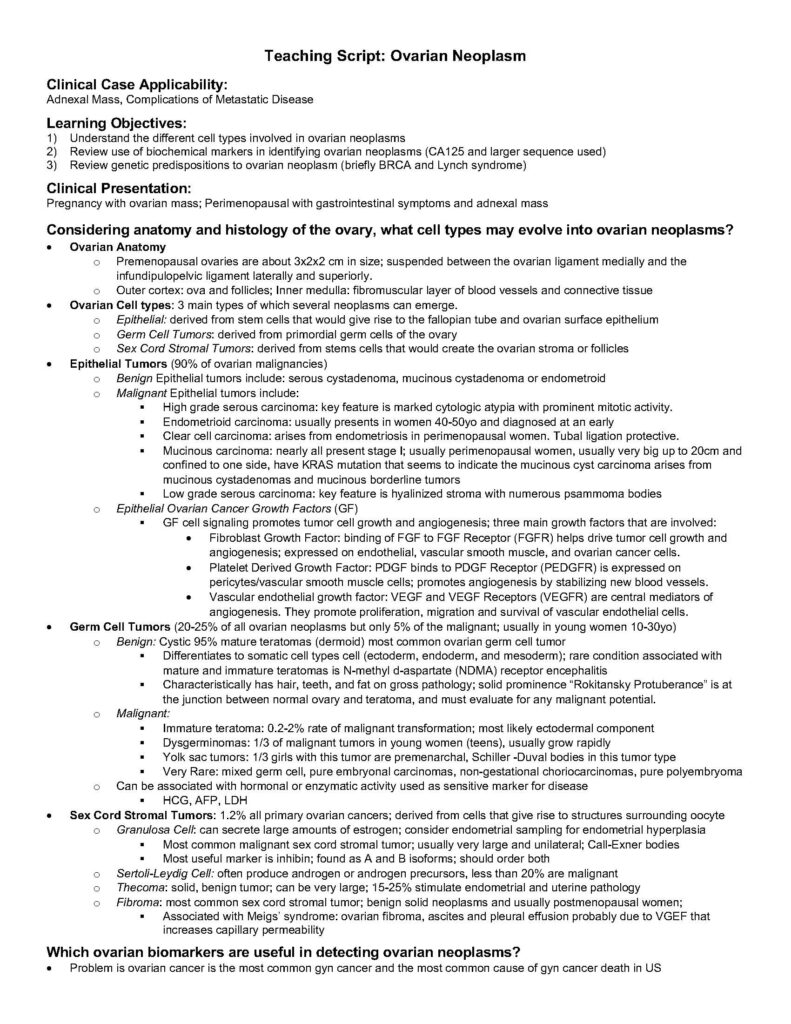
• Ovarian Cell types: 3 main types of which several neoplasms can emerge.
o Epithelial: derived from stem cells that would give rise to the fallopian tube and ovarian surface epithelium
o Germ Cell Tumors: derived from primordial germ cells of the ovary
o Sex Cord Stromal Tumors: derived from stems cells that would create the ovarian stroma or follicles
• Epithelial Tumors (90% of ovarian malignancies)
o Benign Epithelial tumors include: serous cystadenoma, mucinous cystadenoma or endometroid
o Malignant Epithelial tumors include:
§ High grade serous carcinoma: key feature is marked cytologic atypia with prominent mitotic activity.
§ Endometrioid carcinoma: usually presents in women 40-50yo and diagnosed at an early
§ Clear cell carcinoma: arises from endometriosis in perimenopausal women. Tubal ligation protective.
§ Mucinous carcinoma: nearly all present stage I; usually perimenopausal women, usually very big up to 20cm and
confined to one side, have KRAS mutation that seems to indicate the mucinous cyst carcinoma arises from
mucinous cystadenomas and mucinous borderline tumors
§ Low grade serous carcinoma: key feature is hyalinized stroma with numerous psammoma bodies
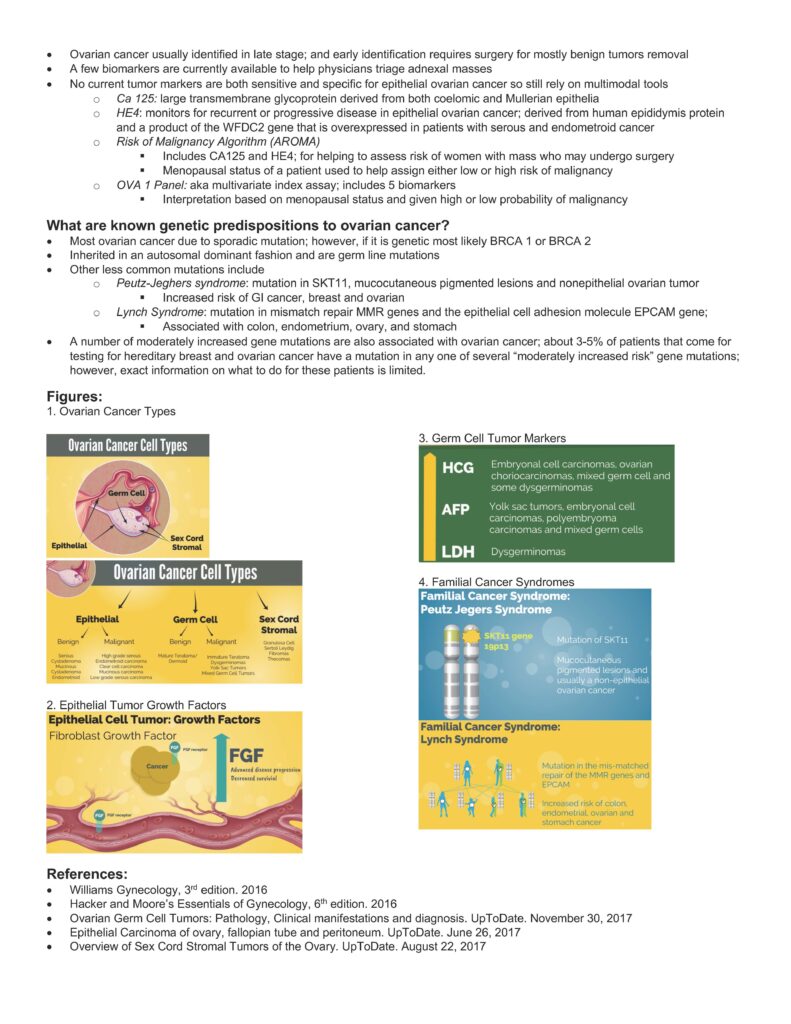
o Epithelial Ovarian Cancer Growth Factors (GF)
§ GF cell signaling promotes tumor cell growth and angiogenesis; three main growth factors that are involved:
• Fibroblast Growth Factor: binding of FGF to FGF Receptor (FGFR) helps drive tumor cell growth and
angiogenesis; expressed on endothelial, vascular smooth muscle, and ovarian cancer cells.
• Platelet Derived Growth Factor: PDGF binds to PDGF Receptor (PEDGFR) is expressed on
pericytes/vascular smooth muscle cells; promotes angiogenesis by stabilizing new blood vessels.
• Vascular endothelial growth factor: VEGF and VEGF Receptors (VEGFR) are central mediators of
angiogenesis. They promote proliferation, migration and survival of vascular endothelial cells.
• Germ Cell Tumors (20-25% of all ovarian neoplasms but only 5% of the malignant; usually in young women 10-30yo)
o Benign: Cystic 95% mature teratomas (dermoid) most common ovarian germ cell tumor
§ Differentiates to somatic cell types cell (ectoderm, endoderm, and mesoderm); rare condition associated with
mature and immature teratomas is N-methyl d-aspartate (NDMA) receptor encephalitis
§ Characteristically has hair, teeth, and fat on gross pathology; solid prominence “Rokitansky Protuberance” is at
the junction between normal ovary and teratoma, and must evaluate for any malignant potential.
o Malignant:
§ Immature teratoma: 0.2-2% rate of malignant transformation; most likely ectodermal component
§ Dysgerminomas: 1/3 of malignant tumors in young women (teens), usually grow rapidly
§ Yolk sac tumors: 1/3 girls with this tumor are premenarchal, Schiller -Duval bodies in this tumor type
§ Very Rare: mixed germ cell, pure embryonal carcinomas, non-gestational choriocarcinomas, pure polyembryoma
o Can be associated with hormonal or enzymatic activity used as sensitive marker for disease
§ HCG, AFP, LDH
• Sex Cord Stromal Tumors: 1.2% all primary ovarian cancers; derived from cells that give rise to structures surrounding oocyte
o Granulosa Cell: can secrete large amounts of estrogen; consider endometrial sampling for endometrial hyperplasia
§ Most common malignant sex cord stromal tumor; usually very large and unilateral; Call-Exner bodies
§ Most useful marker is inhibin; found as A and B isoforms; should order both
o Sertoli-Leydig Cell: often produce androgen or androgen precursors, less than 20% are malignant
o Thecoma: solid, benign tumor; can be very large; 15-25% stimulate endometrial and uterine pathology
o Fibroma: most common sex cord stromal tumor; benign solid neoplasms and usually postmenopausal women;
§ Associated with Meigs’ syndrome: ovarian fibroma, ascites and pleural effusion probably due to VGEF that
increases capillary permeability
Which ovarian biomarkers are useful in detecting ovarian neoplasms?
• Problem is ovarian cancer is the most common gyn cancer and the most common cause of gyn cancer death in US
• Ovarian cancer usually identified in late stage; and early identification requires surgery for mostly benign tumors removal
• A few biomarkers are currently available to help physicians triage adnexal masses
• No current tumor markers are both sensitive and specific for epithelial ovarian cancer so still rely on multimodal tools
o Ca 125: large transmembrane glycoprotein derived from both coelomic and Mullerian epithelia
o HE4: monitors for recurrent or progressive disease in epithelial ovarian cancer; derived from human epididymis protein
and a product of the WFDC2 gene that is overexpressed in patients with serous and endometroid cancer
o Risk of Malignancy Algorithm (AROMA)
§ Includes CA125 and HE4; for helping to assess risk of women with mass who may undergo surgery
§ Menopausal status of a patient used to help assign either low or high risk of malignancy
o OVA 1 Panel: aka multivariate index assay; includes 5 biomarkers
§ Interpretation based on menopausal status and given high or low probability of malignancy
What are known genetic predispositions to ovarian cancer?
• Most ovarian cancer due to sporadic mutation; however, if it is genetic most likely BRCA 1 or BRCA 2
• Inherited in an autosomal dominant fashion and are germ line mutations
• Other less common mutations include
o Peutz-Jeghers syndrome: mutation in SKT11, mucocutaneous pigmented lesions and nonepithelial ovarian tumor
§ Increased risk of GI cancer, breast and ovarian
o Lynch Syndrome: mutation in mismatch repair MMR genes and the epithelial cell adhesion molecule EPCAM gene;
§ Associated with colon, endometrium, ovary, and stomach
• A number of moderately increased gene mutations are also associated with ovarian cancer; about 3-5% of patients that come for
testing for hereditary breast and ovarian cancer have a mutation in any one of several “moderately increased risk” gene mutations;
however, exact information on what to do for these patients is limited.
Figures:
1. Ovarian Cancer Types
2. Epithelial Tumor Growth Factors
3. Germ Cell Tumor Markers
4. Familial Cancer Syndromes
References:
• Williams Gynecology, 3rd edition. 2016
• Hacker and Moore’s Essentials of Gynecology, 6th edition. 2016
• Ovarian Germ Cell Tumors: Pathology, Clinical manifestations and diagnosis. UpToDate. November 30, 2017
• Epithelial Carcinoma of ovary, fallopian tube and peritoneum. UpToDate. June 26, 2017
• Overview of Sex Cord Stromal Tumors of the Ovary. UpToDate. August 22, 2017