Pelvic Anatomy
Duration 11:23
Teaching Script: Pelvic Anatomy
Clinical Case Applicability:
Obstetric planning, Gynecologic surgeries, Foundation for Clinical Evaluation
Learning Objectives:
1. Understand the major anatomical landmarks of the female pelvis
2. Apply concepts of basic anatomy to clinical cases
3. Understand how anatomy changes due to patient position and habitus
Clinical Presentation:
Obstructed labor, Uterine prolapse, Hysterectomy following multiple abdominal surgeries, Anesthesia for vaginal lacerations after
childbirth, Ectopic pregnancy
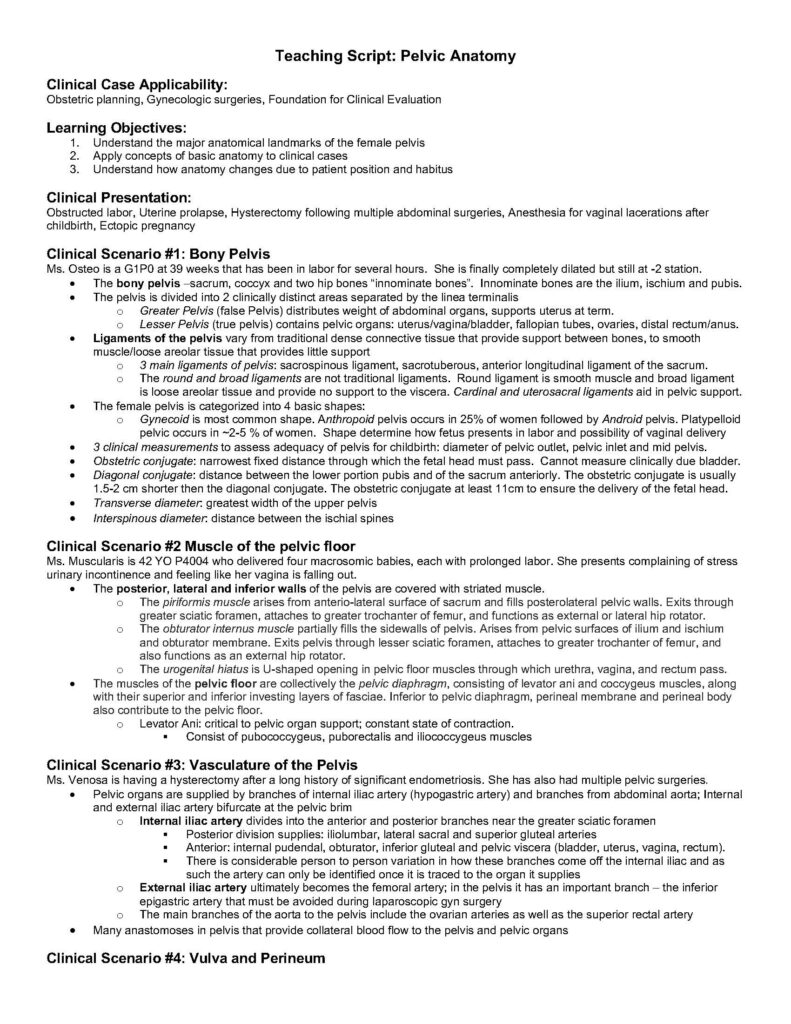
Clinical Scenario #1: Bony Pelvis
Ms. Osteo is a G1P0 at 39 weeks that has been in labor for several hours. She is finally completely dilated but still at -2 station.
• The bony pelvis –sacrum, coccyx and two hip bones “innominate bones”. Innominate bones are the ilium, ischium and pubis.
• The pelvis is divided into 2 clinically distinct areas separated by the linea terminalis
o Greater Pelvis (false Pelvis) distributes weight of abdominal organs, supports uterus at term.
o Lesser Pelvis (true pelvis) contains pelvic organs: uterus/vagina/bladder, fallopian tubes, ovaries, distal rectum/anus.
• Ligaments of the pelvis vary from traditional dense connective tissue that provide support between bones, to smooth
muscle/loose areolar tissue that provides little support
o 3 main ligaments of pelvis: sacrospinous ligament, sacrotuberous, anterior longitudinal ligament of the sacrum.
o The round and broad ligaments are not traditional ligaments. Round ligament is smooth muscle and broad ligament
is loose areolar tissue and provide no support to the viscera. Cardinal and uterosacral ligaments aid in pelvic support.
• The female pelvis is categorized into 4 basic shapes:
o Gynecoid is most common shape. Anthropoid pelvis occurs in 25% of women followed by Android pelvis. Platypelloid
pelvic occurs in ~2-5 % of women. Shape determine how fetus presents in labor and possibility of vaginal delivery
• 3 clinical measurements to assess adequacy of pelvis for childbirth: diameter of pelvic outlet, pelvic inlet and mid pelvis.
• Obstetric conjugate: narrowest fixed distance through which the fetal head must pass. Cannot measure clinically due bladder.
• Diagonal conjugate: distance between the lower portion pubis and of the sacrum anteriorly. The obstetric conjugate is usually
1.5-2 cm shorter then the diagonal conjugate. The obstetric conjugate at least 11cm to ensure the delivery of the fetal head.
• Transverse diameter: greatest width of the upper pelvis
• Interspinous diameter: distance between the ischial spines
Clinical Scenario #2 Muscle of the pelvic floor
Ms. Muscularis is 42 YO P4004 who delivered four macrosomic babies, each with prolonged labor. She presents complaining of stress
urinary incontinence and feeling like her vagina is falling out.
• The posterior, lateral and inferior walls of the pelvis are covered with striated muscle.
o The piriformis muscle arises from anterio-lateral surface of sacrum and fills posterolateral pelvic walls. Exits through
greater sciatic foramen, attaches to greater trochanter of femur, and functions as external or lateral hip rotator.
o The obturator internus muscle partially fills the sidewalls of pelvis. Arises from pelvic surfaces of ilium and ischium
and obturator membrane. Exits pelvis through lesser sciatic foramen, attaches to greater trochanter of femur, and
also functions as an external hip rotator.
o The urogenital hiatus is U-shaped opening in pelvic floor muscles through which urethra, vagina, and rectum pass.
• The muscles of the pelvic floor are collectively the pelvic diaphragm, consisting of levator ani and coccygeus muscles, along
with their superior and inferior investing layers of fasciae. Inferior to pelvic diaphragm, perineal membrane and perineal body
also contribute to the pelvic floor.
o Levator Ani: critical to pelvic organ support; constant state of contraction.
§ Consist of pubococcygeus, puborectalis and iliococcygeus muscles
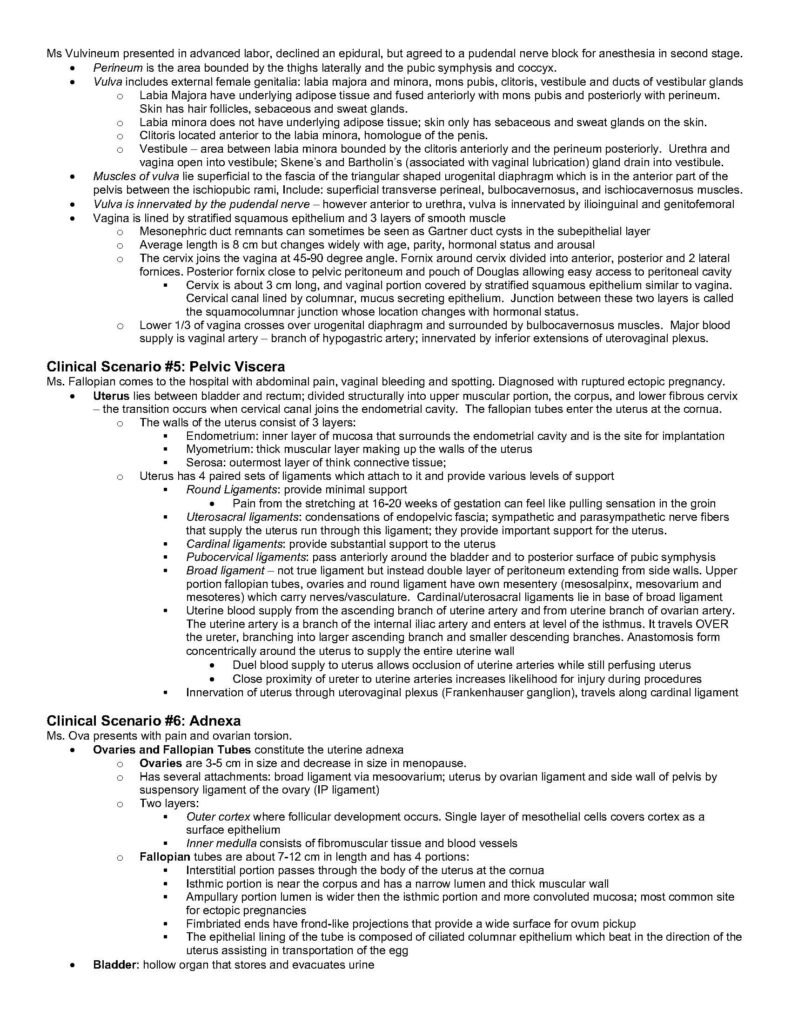
Clinical Scenario #3: Vasculature of the Pelvis
Ms. Venosa is having a hysterectomy after a long history of significant endometriosis. She has also had multiple pelvic surgeries.
• Pelvic organs are supplied by branches of internal iliac artery (hypogastric artery) and branches from abdominal aorta; Internal
and external iliac artery bifurcate at the pelvic brim
o Internal iliac artery divides into the anterior and posterior branches near the greater sciatic foramen
§ Posterior division supplies: iliolumbar, lateral sacral and superior gluteal arteries
§ Anterior: internal pudendal, obturator, inferior gluteal and pelvic viscera (bladder, uterus, vagina, rectum).
§ There is considerable person to person variation in how these branches come off the internal iliac and as
such the artery can only be identified once it is traced to the organ it supplies
o External iliac artery ultimately becomes the femoral artery; in the pelvis it has an important branch – the inferior
epigastric artery that must be avoided during laparoscopic gyn surgery
o The main branches of the aorta to the pelvis include the ovarian arteries as well as the superior rectal artery
• Many anastomoses in pelvis that provide collateral blood flow to the pelvis and pelvic organs
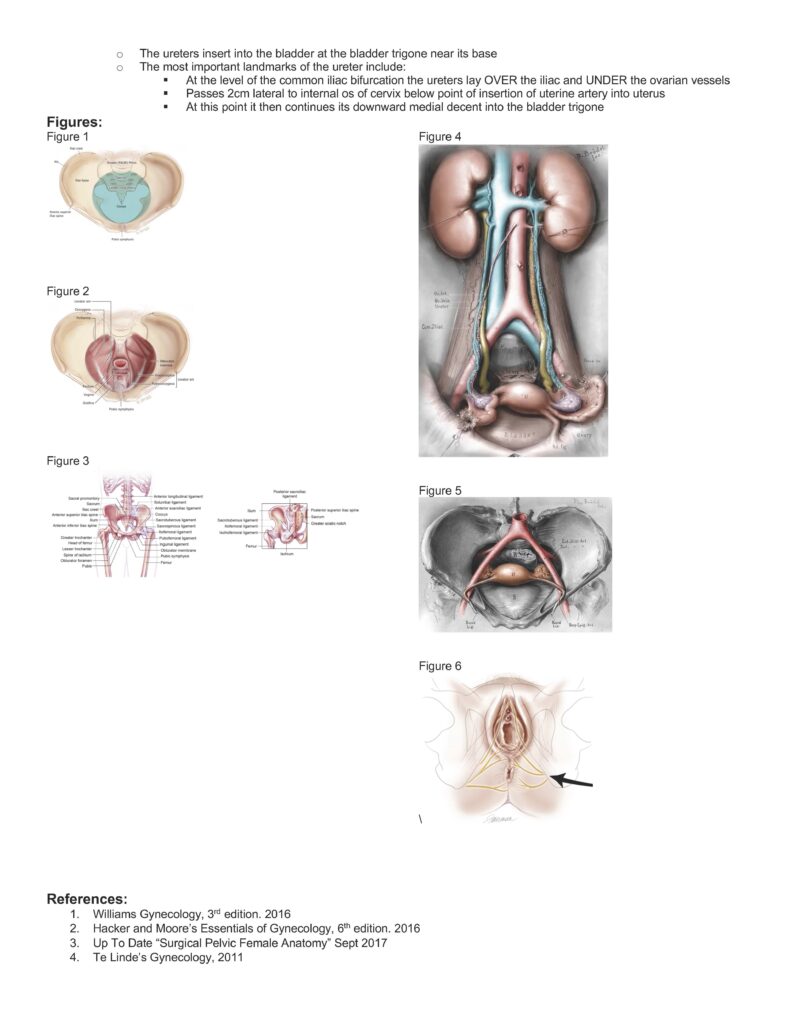
Clinical Scenario #4: Vulva and Perineum
Ms Vulvineum presented in advanced labor, declined an epidural, but agreed to a pudendal nerve block for anesthesia in second stage.
• Perineum is the area bounded by the thighs laterally and the pubic symphysis and coccyx.
• Vulva includes external female genitalia: labia majora and minora, mons pubis, clitoris, vestibule and ducts of vestibular glands
o Labia Majora have underlying adipose tissue and fused anteriorly with mons pubis and posteriorly with perineum.
Skin has hair follicles, sebaceous and sweat glands.
o Labia minora does not have underlying adipose tissue; skin only has sebaceous and sweat glands on the skin.
o Clitoris located anterior to the labia minora, homologue of the penis.
o Vestibule – area between labia minora bounded by the clitoris anteriorly and the perineum posteriorly. Urethra and
vagina open into vestibule; Skene’s and Bartholin’s (associated with vaginal lubrication) gland drain into vestibule.
• Muscles of vulva lie superficial to the fascia of the triangular shaped urogenital diaphragm which is in the anterior part of the
pelvis between the ischiopubic rami, Include: superficial transverse perineal, bulbocavernosus, and ischiocavernosus muscles.
• Vulva is innervated by the pudendal nerve – however anterior to urethra, vulva is innervated by ilioinguinal and genitofemoral
• Vagina is lined by stratified squamous epithelium and 3 layers of smooth muscle
o Mesonephric duct remnants can sometimes be seen as Gartner duct cysts in the subepithelial layer
o Average length is 8 cm but changes widely with age, parity, hormonal status and arousal
o The cervix joins the vagina at 45-90 degree angle. Fornix around cervix divided into anterior, posterior and 2 lateral
fornices. Posterior fornix close to pelvic peritoneum and pouch of Douglas allowing easy access to peritoneal cavity
§ Cervix is about 3 cm long, and vaginal portion covered by stratified squamous epithelium similar to vagina.
Cervical canal lined by columnar, mucus secreting epithelium. Junction between these two layers is called
the squamocolumnar junction whose location changes with hormonal status.
o Lower 1/3 of vagina crosses over urogenital diaphragm and surrounded by bulbocavernosus muscles. Major blood
supply is vaginal artery – branch of hypogastric artery; innervated by inferior extensions of uterovaginal plexus.
Clinical Scenario #5: Pelvic Viscera
Ms. Fallopian comes to the hospital with abdominal pain, vaginal bleeding and spotting. Diagnosed with ruptured ectopic pregnancy.
• Uterus lies between bladder and rectum; divided structurally into upper muscular portion, the corpus, and lower fibrous cervix
– the transition occurs when cervical canal joins the endometrial cavity. The fallopian tubes enter the uterus at the cornua.
o The walls of the uterus consist of 3 layers:
§ Endometrium: inner layer of mucosa that surrounds the endometrial cavity and is the site for implantation
§ Myometrium: thick muscular layer making up the walls of the uterus
§ Serosa: outermost layer of think connective tissue;
o Uterus has 4 paired sets of ligaments which attach to it and provide various levels of support
§ Round Ligaments: provide minimal support
• Pain from the stretching at 16-20 weeks of gestation can feel like pulling sensation in the groin
§ Uterosacral ligaments: condensations of endopelvic fascia; sympathetic and parasympathetic nerve fibers
that supply the uterus run through this ligament; they provide important support for the uterus.
§ Cardinal ligaments: provide substantial support to the uterus
§ Pubocervical ligaments: pass anteriorly around the bladder and to posterior surface of pubic symphysis
§ Broad ligament – not true ligament but instead double layer of peritoneum extending from side walls. Upper
portion fallopian tubes, ovaries and round ligament have own mesentery (mesosalpinx, mesovarium and
mesoteres) which carry nerves/vasculature. Cardinal/uterosacral ligaments lie in base of broad ligament
§ Uterine blood supply from the ascending branch of uterine artery and from uterine branch of ovarian artery.
The uterine artery is a branch of the internal iliac artery and enters at level of the isthmus. It travels OVER
the ureter, branching into larger ascending branch and smaller descending branches. Anastomosis form
concentrically around the uterus to supply the entire uterine wall
• Duel blood supply to uterus allows occlusion of uterine arteries while still perfusing uterus
• Close proximity of ureter to uterine arteries increases likelihood for injury during procedures
§ Innervation of uterus through uterovaginal plexus (Frankenhauser ganglion), travels along cardinal ligament
Clinical Scenario #6: Adnexa
Ms. Ova presents with pain and ovarian torsion.
• Ovaries and Fallopian Tubes constitute the uterine adnexa
o Ovaries are 3-5 cm in size and decrease in size in menopause.
o Has several attachments: broad ligament via mesoovarium; uterus by ovarian ligament and side wall of pelvis by
suspensory ligament of the ovary (IP ligament)
o Two layers:
§ Outer cortex where follicular development occurs. Single layer of mesothelial cells covers cortex as a
surface epithelium
§ Inner medulla consists of fibromuscular tissue and blood vessels
o Fallopian tubes are about 7-12 cm in length and has 4 portions:
§ Interstitial portion passes through the body of the uterus at the cornua
§ Isthmic portion is near the corpus and has a narrow lumen and thick muscular wall
§ Ampullary portion lumen is wider then the isthmic portion and more convoluted mucosa; most common site
for ectopic pregnancies
§ Fimbriated ends have frond-like projections that provide a wide surface for ovum pickup
§ The epithelial lining of the tube is composed of ciliated columnar epithelium which beat in the direction of the
uterus assisting in transportation of the egg
• Bladder: hollow organ that stores and evacuates urine
o The ureters insert into the bladder at the bladder trigone near its base
o The most important landmarks of the ureter include:
§ At the level of the common iliac bifurcation the ureters lay OVER the iliac and UNDER the ovarian vessels
§ Passes 2cm lateral to internal os of cervix below point of insertion of uterine artery into uterus
§ At this point it then continues its downward medial decent into the bladder trigone
Figures:
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
\
References:
1. Williams Gynecology, 3rd edition. 2016
2. Hacker and Moore’s Essentials of Gynecology, 6th edition. 2016
3. Up To Date “Surgical Pelvic Female Anatomy” Sept 2017
4. Te Linde’s Gynecology, 2011