Postpartum Depression
Duration 9:17
Postpartum Depression
Liang A
Clinical Cases Applicability: Antepartum mood disorders, postpartum blues, postpartum depression
Learning Objectives:
1. Understand the neurobiological mechanisms underlying postpartum depression
2. Describe the pharmacology of SSRIs
What are some sex differences in depression?
-Women 2x more likely to develop depression, greatest difference in reproductive years – suggests sex hormones (estrogen, progesterone, oxytocin) and reproductive events play some role in etiology of depression
What is the definition of PDD? prevalence? Risk factors? Natural history?
-DSM 5 defines peri-partum depression as symptom onset during pregnancy or <4 weeks PP – but greatest incidence of new PPD occurs 2-3 months postpartum, and can occur within 1 year
-Prevalence ~10-15%
-Risk factors: antenatal depression (↑ prevalence in 2nd/3rd trimesters) & depression prior to pregnancy; stressful life events (marital conflict, emigration), poor social & financial support
– Often remits on its own within 12 months after giving birth, 6x increased risk for depression later in life
What are proposed neurobiological mechanisms underlying PPD? Pathogenesis unknown
Genetics: increased risk with family history of PPD
Abnormal neurotransmitter levels/activity: ↑ brain monoamine oxidase ↑ metabolism of neurotransmitters such as dopamine, norepinephrine, serotonin more rapid depletion of these neurotransmitters depression
Significant changes in neural activity in brain regions important for self-regulation, empathy & emotion; fMRI studies identify brain regions affected by postpartum depression at rest and in response to infant or non-infant emotional cues
–Decreased corticortical and corticolimbic connectivity
-Weaker connectivity among the amygdala (processes emotions), anterior cingulate cortex (connects the “emotional” limbic system and the “cognitive” prefrontal cortex), dorsal lateral prefrontal cortex (working memory) & hippocampus (long term memory, emotional responses)
-decreased connectivity between the amygdala and right insular cortex w/ positive infant cues
Abnormal growth factors: ↓ Brain-derived neurotrophic factor (supports differentiation, maturation and survival of neurons) concentrations in PPD
What hormones may play a role in PPD? women with a predisposition for depression may be more sensitive to large fluctuations in steroid hormone levels
Estradiol: estradiol levels continue to ↑ in 3rd trimester, but drop dramatically after birth “estradiol-withdrawal state”
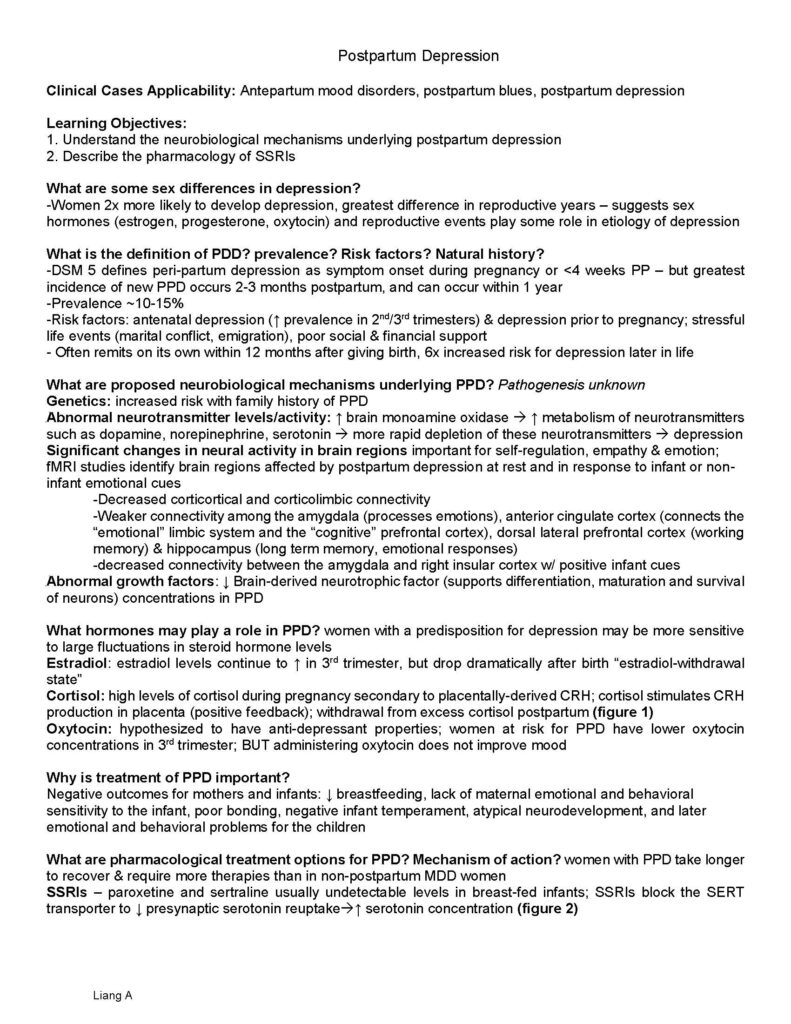
Cortisol: high levels of cortisol during pregnancy secondary to placentally-derived CRH; cortisol stimulates CRH production in placenta (positive feedback); withdrawal from excess cortisol postpartum (figure 1)
Oxytocin: hypothesized to have anti-depressant properties; women at risk for PPD have lower oxytocin concentrations in 3rd trimester; BUT administering oxytocin does not improve mood
Why is treatment of PPD important?
Negative outcomes for mothers and infants: ↓ breastfeeding, lack of maternal emotional and behavioral sensitivity to the infant, poor bonding, negative infant temperament, atypical neurodevelopment, and later emotional and behavioral problems for the children
What are pharmacological treatment options for PPD? Mechanism of action? women with PPD take longer to recover & require more therapies than in non-postpartum MDD women
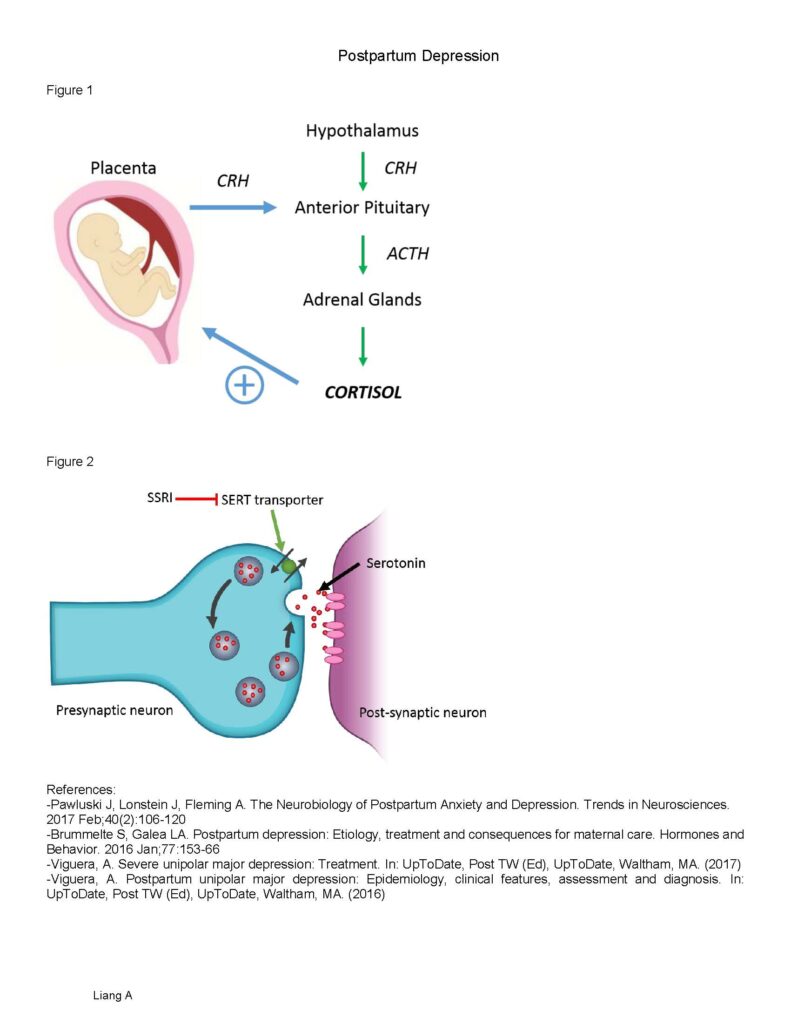
SSRIs – paroxetine and sertraline usually undetectable levels in breast-fed infants; SSRIs block the SERT transporter to ↓ presynaptic serotonin reuptake↑ serotonin concentration (figure 2) Postpartum Depression
Liang A
Figure 1
Figure 2
References:
-Pawluski J, Lonstein J, Fleming A. The Neurobiology of Postpartum Anxiety and Depression. Trends in Neurosciences. 2017 Feb;40(2):106-120
-Brummelte S, Galea LA. Postpartum depression: Etiology, treatment and consequences for maternal care. Hormones and Behavior. 2016 Jan;77:153-66
-Viguera, A. Severe unipolar major depression: Treatment. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2017)
-Viguera, A. Postpartum unipolar major depression: Epidemiology, clinical features, assessment and diagnosis. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2016)