Urinary Incontinence
Duration 9:46
Urinary Incontinence
Liang A
Clinical Cases Applicability: Urinary incontinence, urinary retention
Learning Objectives:
1) Describe the anatomy of the bladder
2) Understand the physiology of normal bladder filling, emptying and continence
3) Understand the autonomic control of the bladder
4) Understand the pathophysiology of urinary incontinence
5) Describe the pharmacology of medications for urge incontinence
Describe the layers of the bladder wall:
1)Mucosa – consists of transitional cell epithelium and lamina propria 2)Submucosa 3)Muscularis – detrusor composed of 3 smooth-muscle “plexiform” layers allow for rapid expansion 4)Adventita
What is unique about the transitional cell epithelium? “Umbrella” cell layer – stretches & thins with bladder filling; impermeable to provide urine-plasma barrier; covering the lining is a glycosaminoglycan (GAG) layer prohibits bacterial adherence and acts as a protective barrier
What are the components of the peripheral nervous system?
Somatic: innervates striated muscle, VOLUNTARY movements
Autonomic: innervates smooth muscle, INVOLUNTARY movements
Sympathetic “fight or flight”: acts through epinephrine & norepinephrine on α and β adrenergic receptors
Parasympathetic “rest and digest”: acts through acetycholine (Ach) binding to muscarinic or nicotinic receptors
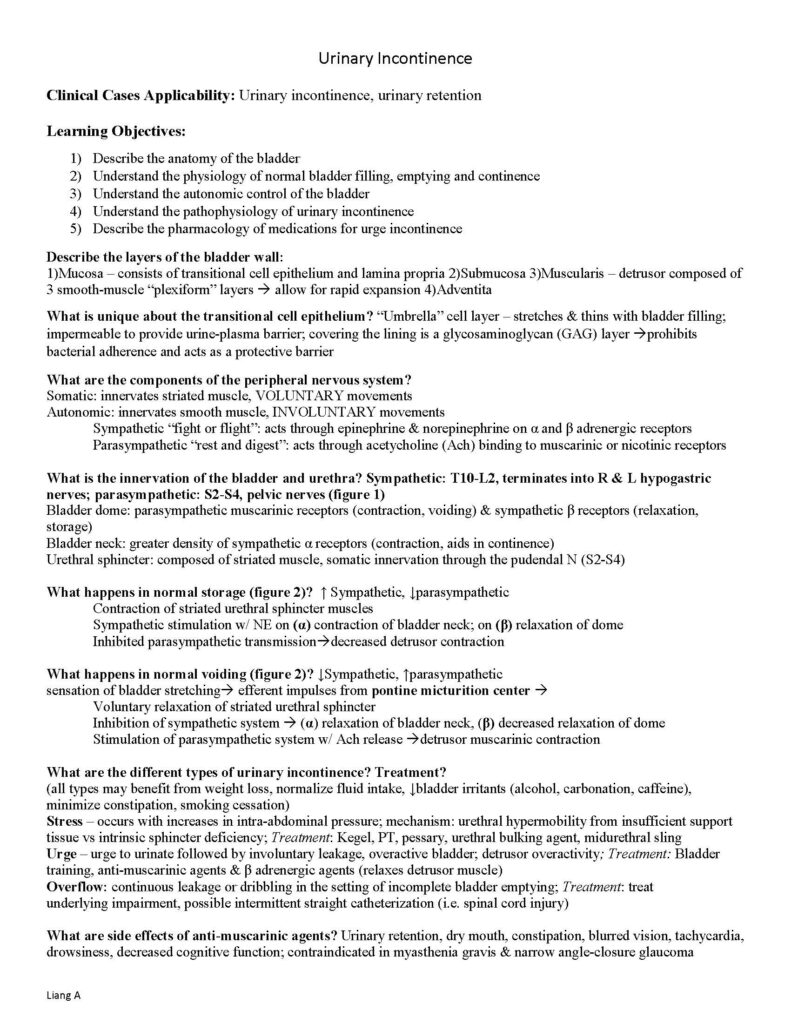
What is the innervation of the bladder and urethra? Sympathetic: T10-L2, terminates into R & L hypogastric nerves; parasympathetic: S2-S4, pelvic nerves (figure 1)
Bladder dome: parasympathetic muscarinic receptors (contraction, voiding) & sympathetic β receptors (relaxation, storage)
Bladder neck: greater density of sympathetic α receptors (contraction, aids in continence)
Urethral sphincter: composed of striated muscle, somatic innervation through the pudendal N (S2-S4)
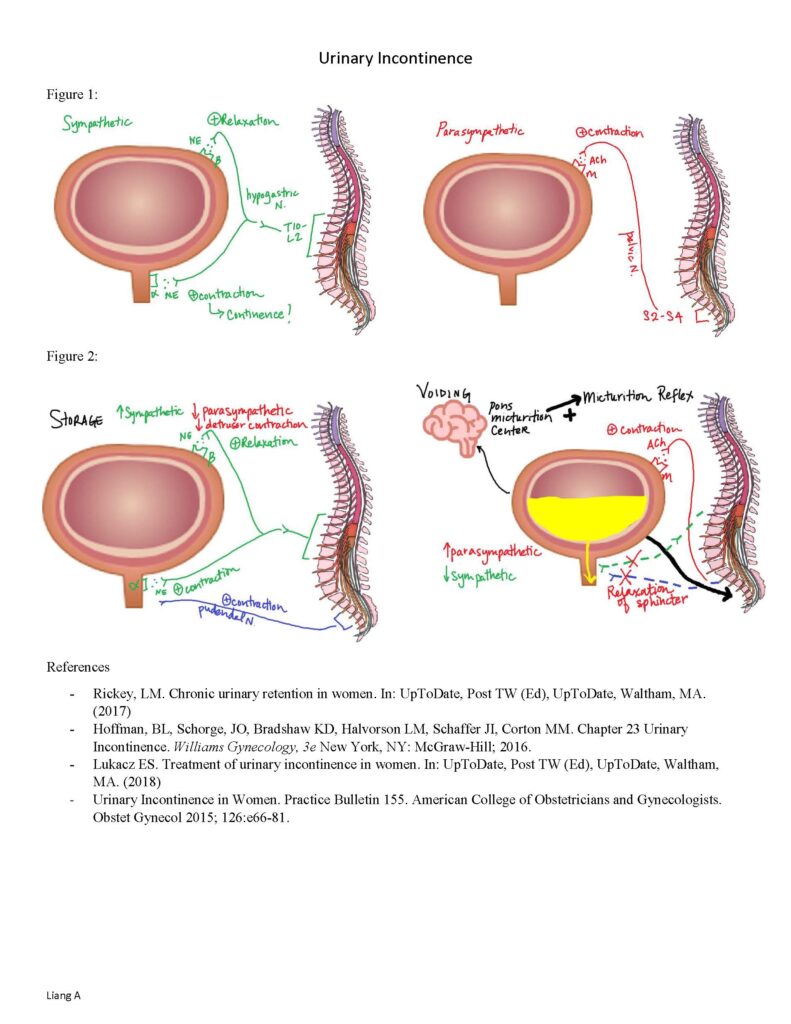
What happens in normal storage (figure 2)? ↑ Sympathetic, ↓parasympathetic
Contraction of striated urethral sphincter muscles
Sympathetic stimulation w/ NE on (α) contraction of bladder neck; on (β) relaxation of dome
Inhibited parasympathetic transmissiondecreased detrusor contraction
What happens in normal voiding (figure 2)? ↓Sympathetic, ↑parasympathetic
sensation of bladder stretching efferent impulses from pontine micturition center
Voluntary relaxation of striated urethral sphincter
Inhibition of sympathetic system (α) relaxation of bladder neck, (β) decreased relaxation of dome
Stimulation of parasympathetic system w/ Ach release detrusor muscarinic contraction
What are the different types of urinary incontinence? Treatment?
(all types may benefit from weight loss, normalize fluid intake, ↓bladder irritants (alcohol, carbonation, caffeine), minimize constipation, smoking cessation)
Stress – occurs with increases in intra-abdominal pressure; mechanism: urethral hypermobility from insufficient support tissue vs intrinsic sphincter deficiency; Treatment: Kegel, PT, pessary, urethral bulking agent, midurethral sling
Urge – urge to urinate followed by involuntary leakage, overactive bladder; detrusor overactivity; Treatment: Bladder
training, anti-muscarinic agents & β adrenergic agents (relaxes detrusor muscle)
Overflow: continuous leakage or dribbling in the setting of incomplete bladder emptying; Treatment: treat
underlying impairment, possible intermittent straight catheterization (i.e. spinal cord injury)
What are side effects of anti-muscarinic agents? Urinary retention, dry mouth, constipation, blurred vision, tachycardia, drowsiness, decreased cognitive function; contraindicated in myasthenia gravis & narrow angle-closure glaucoma Urinary Incontinence
Liang A
Figure 1:
Figure 2:
References
– Rickey, LM. Chronic urinary retention in women. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2017)
– Hoffman, BL, Schorge, JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Chapter 23 Urinary Incontinence. Williams Gynecology, 3e New York, NY: McGraw-Hill; 2016.
– Lukacz ES. Treatment of urinary incontinence in women. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2018)
– Urinary Incontinence in Women. Practice Bulletin 155. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015; 126:e66-81.