Uterine Atony
Duration 11:41
Teaching Script: Uterine Atony
Clinical Cases Applicability: Postpartum hemorrhage (PPH), post-abortal hemorrhage
Learning Objectives:
• Understand the mechanism of uterine muscle architecture and contractility
• Describe how risk factors for uterine atony interfere with myometrial contraction
• Appreciate the mechanism of action and pharmacology of uterotonic agents
• Describe the physiologic mechanism by which mechanical therapy improves uterine tone
Clinical Presentation: PPH following prolonged labor and chorioamnionitis, delivery of multiple gestation
How is uterine contractility controlled in vivo?
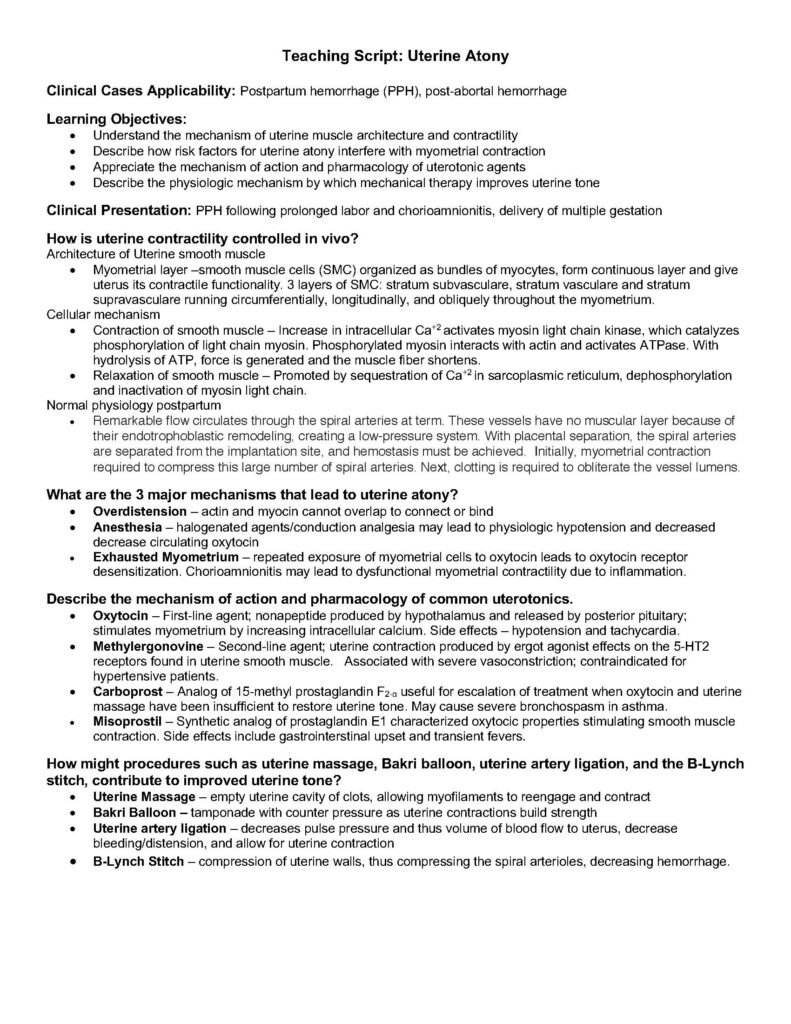
Architecture of Uterine smooth muscle
• Myometrial layer –smooth muscle cells (SMC) organized as bundles of myocytes, form continuous layer and give
uterus its contractile functionality. 3 layers of SMC: stratum subvasculare, stratum vasculare and stratum
supravasculare running circumferentially, longitudinally, and obliquely throughout the myometrium.
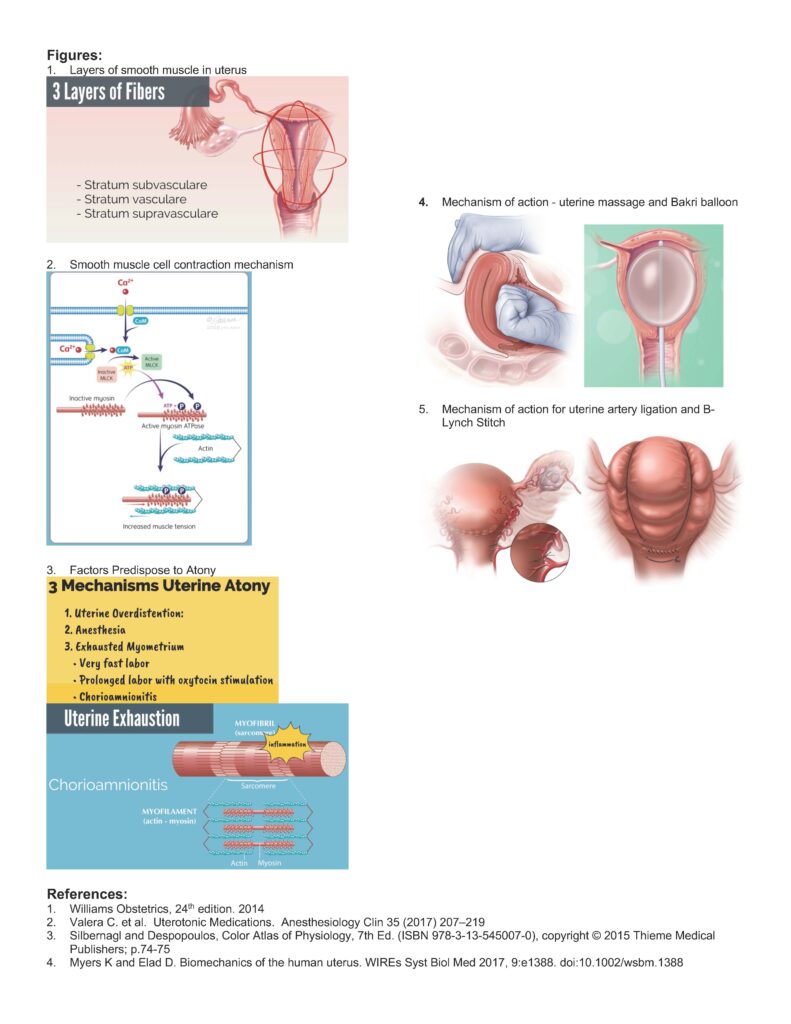
Cellular mechanism
• Contraction of smooth muscle – Increase in intracellular Ca+2 activates myosin light chain kinase, which catalyzes
phosphorylation of light chain myosin. Phosphorylated myosin interacts with actin and activates ATPase. With
hydrolysis of ATP, force is generated and the muscle fiber shortens.
• Relaxation of smooth muscle – Promoted by sequestration of Ca+2 in sarcoplasmic reticulum, dephosphorylation
and inactivation of myosin light chain.
Normal physiology postpartum
• Remarkable flow circulates through the spiral arteries at term. These vessels have no muscular layer because of
their endotrophoblastic remodeling, creating a low-pressure system. With placental separation, the spiral arteries
are separated from the implantation site, and hemostasis must be achieved. Initially, myometrial contraction
required to compress this large number of spiral arteries. Next, clotting is required to obliterate the vessel lumens.
What are the 3 major mechanisms that lead to uterine atony?
• Overdistension – actin and myocin cannot overlap to connect or bind
• Anesthesia – halogenated agents/conduction analgesia may lead to physiologic hypotension and decreased
decrease circulating oxytocin
• Exhausted Myometrium – repeated exposure of myometrial cells to oxytocin leads to oxytocin receptor
desensitization. Chorioamnionitis may lead to dysfunctional myometrial contractility due to inflammation.
Describe the mechanism of action and pharmacology of common uterotonics.
• Oxytocin – First-line agent; nonapeptide produced by hypothalamus and released by posterior pituitary;
stimulates myometrium by increasing intracellular calcium. Side effects – hypotension and tachycardia.
• Methylergonovine – Second-line agent; uterine contraction produced by ergot agonist effects on the 5-HT2
receptors found in uterine smooth muscle. Associated with severe vasoconstriction; contraindicated for
hypertensive patients.
• Carboprost – Analog of 15-methyl prostaglandin F2-α useful for escalation of treatment when oxytocin and uterine
massage have been insufficient to restore uterine tone. May cause severe bronchospasm in asthma.
• Misoprostil – Synthetic analog of prostaglandin E1 characterized oxytocic properties stimulating smooth muscle
contraction. Side effects include gastrointerstinal upset and transient fevers.
How might procedures such as uterine massage, Bakri balloon, uterine artery ligation, and the B-Lynch
stitch, contribute to improved uterine tone?
• Uterine Massage – empty uterine cavity of clots, allowing myofilaments to reengage and contract
• Bakri Balloon – tamponade with counter pressure as uterine contractions build strength
• Uterine artery ligation – decreases pulse pressure and thus volume of blood flow to uterus, decrease
bleeding/distension, and allow for uterine contraction
• B-Lynch Stitch – compression of uterine walls, thus compressing the spiral arterioles, decreasing hemorrhage.
Figures:
1. Layers of smooth muscle in uterus
2. Smooth muscle cell contraction mechanism
3. Factors Predispose to Atony
4. Mechanism of action – uterine massage and Bakri balloon
5. Mechanism of action for uterine artery ligation and BLynch
Stitch
References:
1. Williams Obstetrics, 24th edition. 2014
2. Valera C. et al. Uterotonic Medications. Anesthesiology Clin 35 (2017) 207–219
3. Silbernagl and Despopoulos, Color Atlas of Physiology, 7th Ed. (ISBN 978-3-13-545007-0), copyright © 2015 Thieme Medical
Publishers; p.74-75
4. Myers K and Elad D. Biomechanics of the human uterus. WIREs Syst Biol Med 2017, 9:e1388. doi:10.1002/wsbm.1388