Abnormal Placentation
Duration 9:45
Pathophysiology of Abnormal Placentation
Clinical Cases Applicability:
Painless vaginal bleeding in the second or third trimester, Risk with prior cesarean delivery, Placenta accreta, Placenta previa,
Postpartum hemorrhage, Cesarean hysterectomy
Learning Objectives:
1) Understand the role of the embryonic syncytiotrophoblastic and cytotrophoblastic cells in placental development
2) Describe the layers of the chorion and how the fetal placental development affects the maternal surface
3) Appreciate the basic functions of the placenta
4) Understand risk factors and possible pathophysiology of placenta previa or accreta
Clinical Presentation:
Abnormal placentation visualized on second trimester sonogram, Painless vaginal bleeding at 34 weeks gestation
How does the placenta form after embryonic implantation?
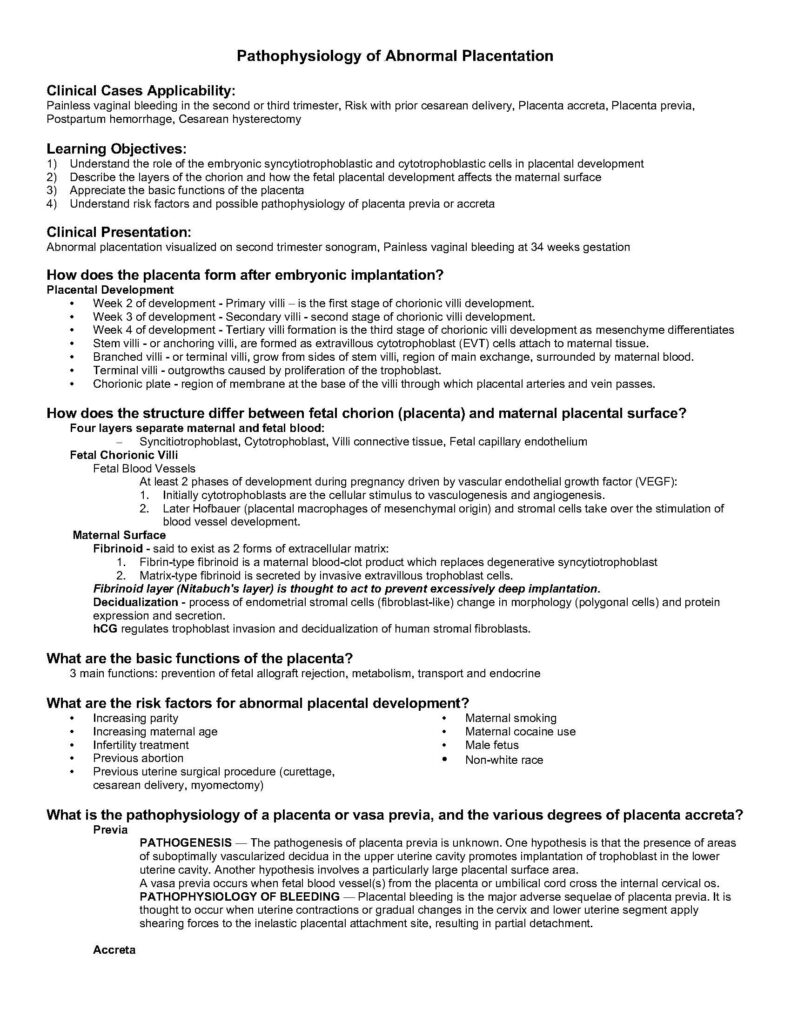
Placental Development
• Week 2 of development – Primary villi – is the first stage of chorionic villi development.
• Week 3 of development – Secondary villi – second stage of chorionic villi development.
• Week 4 of development – Tertiary villi formation is the third stage of chorionic villi development as mesenchyme differentiates
• Stem villi – or anchoring villi, are formed as extravillous cytotrophoblast (EVT) cells attach to maternal tissue.
• Branched villi – or terminal villi, grow from sides of stem villi, region of main exchange, surrounded by maternal blood.
• Terminal villi – outgrowths caused by proliferation of the trophoblast.
• Chorionic plate – region of membrane at the base of the villi through which placental arteries and vein passes.
How does the structure differ between fetal chorion (placenta) and maternal placental surface?
Four layers separate maternal and fetal blood:
– Syncitiotrophoblast, Cytotrophoblast, Villi connective tissue, Fetal capillary endothelium
Fetal Chorionic Villi
Fetal Blood Vessels
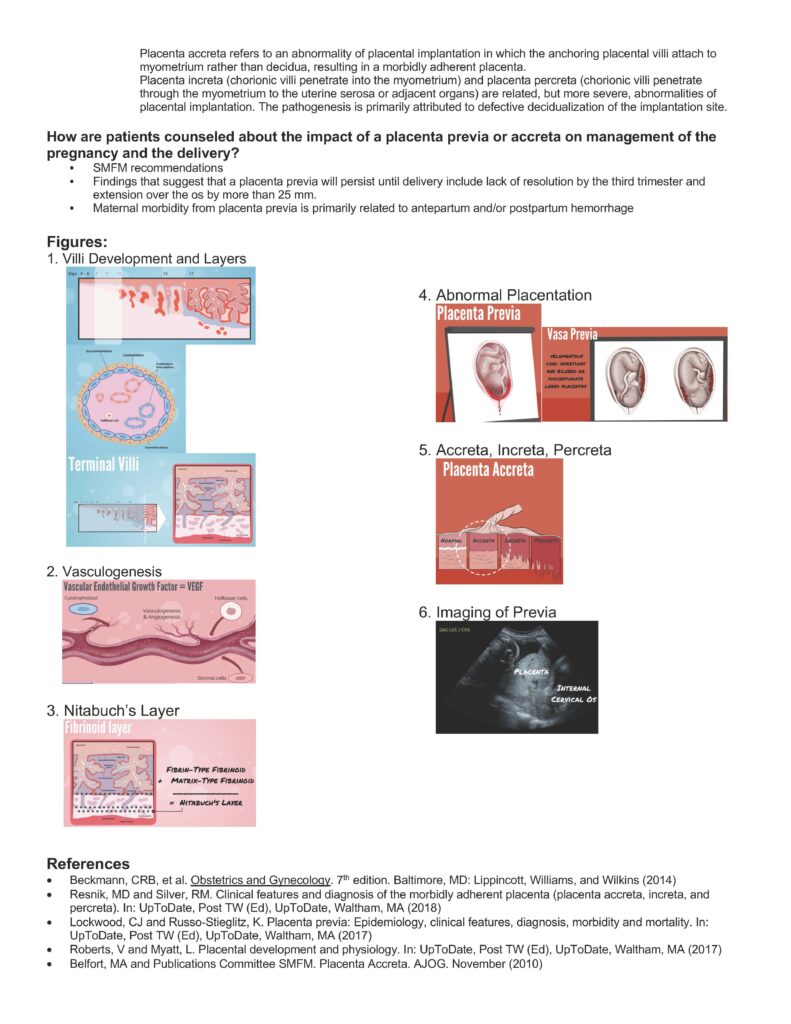
At least 2 phases of development during pregnancy driven by vascular endothelial growth factor (VEGF):
1. Initially cytotrophoblasts are the cellular stimulus to vasculogenesis and angiogenesis.
2. Later Hofbauer (placental macrophages of mesenchymal origin) and stromal cells take over the stimulation of
blood vessel development.
Maternal Surface
Fibrinoid – said to exist as 2 forms of extracellular matrix:
1. Fibrin-type fibrinoid is a maternal blood-clot product which replaces degenerative syncytiotrophoblast
2. Matrix-type fibrinoid is secreted by invasive extravillous trophoblast cells.
Fibrinoid layer (Nitabuch’s layer) is thought to act to prevent excessively deep implantation.
Decidualization – process of endometrial stromal cells (fibroblast-like) change in morphology (polygonal cells) and protein
expression and secretion.
hCG regulates trophoblast invasion and decidualization of human stromal fibroblasts.
What are the basic functions of the placenta?
3 main functions: prevention of fetal allograft rejection, metabolism, transport and endocrine
What are the risk factors for abnormal placental development?
• Increasing parity
• Increasing maternal age
• Infertility treatment
• Previous abortion
• Previous uterine surgical procedure (curettage,
cesarean delivery, myomectomy)
• Maternal smoking
• Maternal cocaine use
• Male fetus
• Non-white race
What is the pathophysiology of a placenta or vasa previa, and the various degrees of placenta accreta?
Previa
PATHOGENESIS — The pathogenesis of placenta previa is unknown. One hypothesis is that the presence of areas
of suboptimally vascularized decidua in the upper uterine cavity promotes implantation of trophoblast in the lower
uterine cavity. Another hypothesis involves a particularly large placental surface area.
A vasa previa occurs when fetal blood vessel(s) from the placenta or umbilical cord cross the internal cervical os.
PATHOPHYSIOLOGY OF BLEEDING — Placental bleeding is the major adverse sequelae of placenta previa. It is
thought to occur when uterine contractions or gradual changes in the cervix and lower uterine segment apply
shearing forces to the inelastic placental attachment site, resulting in partial detachment.
Accreta
Placenta accreta refers to an abnormality of placental implantation in which the anchoring placental villi attach to
myometrium rather than decidua, resulting in a morbidly adherent placenta.
Placenta increta (chorionic villi penetrate into the myometrium) and placenta percreta (chorionic villi penetrate
through the myometrium to the uterine serosa or adjacent organs) are related, but more severe, abnormalities of
placental implantation. The pathogenesis is primarily attributed to defective decidualization of the implantation site.
How are patients counseled about the impact of a placenta previa or accreta on management of the
pregnancy and the delivery?
• SMFM recommendations
• Findings that suggest that a placenta previa will persist until delivery include lack of resolution by the third trimester and
extension over the os by more than 25 mm.
• Maternal morbidity from placenta previa is primarily related to antepartum and/or postpartum hemorrhage
Figures:
1. Villi Development and Layers
2. Vasculogenesis
3. Nitabuch’s Layer
4. Abnormal Placentation
5. Accreta, Increta, Percreta
6. Imaging of Previa
References
• Beckmann, CRB, et al. Obstetrics and Gynecology. 7th edition. Baltimore, MD: Lippincott, Williams, and Wilkins (2014)
• Resnik, MD and Silver, RM. Clinical features and diagnosis of the morbidly adherent placenta (placenta accreta, increta, and
percreta). In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA (2018)
• Lockwood, CJ and Russo-Stieglitz, K. Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. In:
UpToDate, Post TW (Ed), UpToDate, Waltham, MA (2017)
• Roberts, V and Myatt, L. Placental development and physiology. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA (2017)
• Belfort, MA and Publications Committee SMFM. Placenta Accreta. AJOG. November (2010)