Gestational Trophoblastic Disease
Duration 10:02
Gestational Trophoblastic Disease
Liang A
Clinical case applicability: Molar pregnancy, Gestational trophoblastic neoplasia
Learning Objectives:
1). Understand the physiologic stages of fertilization
2). Understand the pathogenesis of complete and partial molar pregnancy
3). Describe the differences in morphology between complete and molar pregnancy
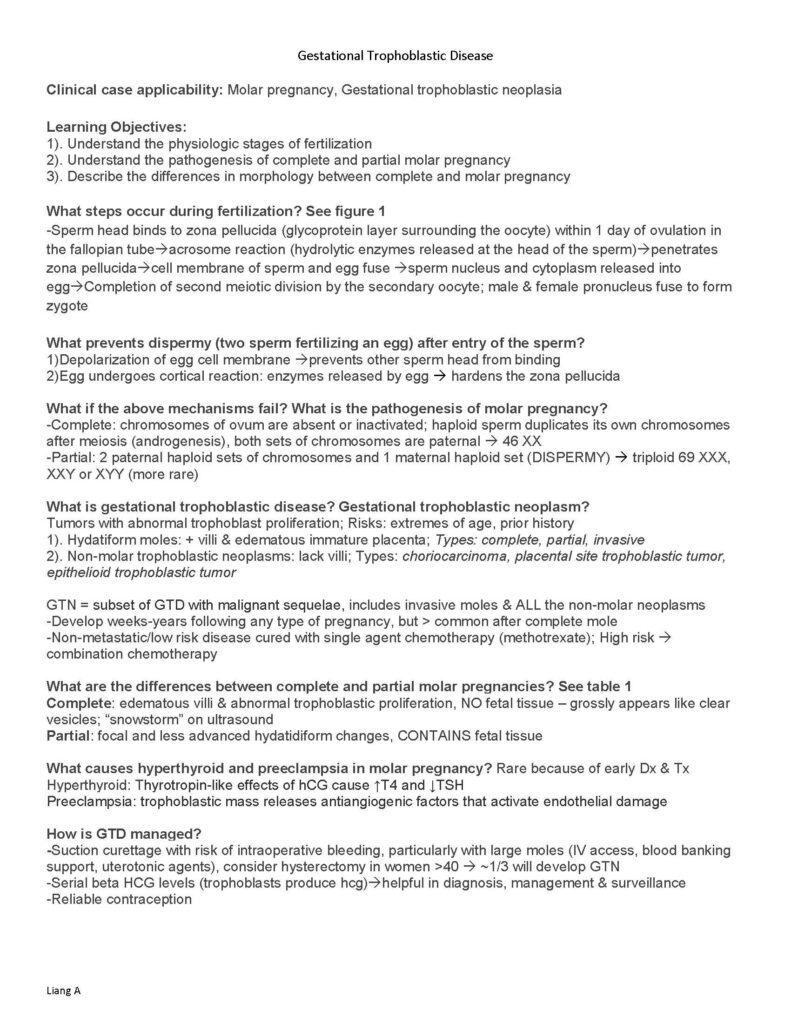
What steps occur during fertilization? See figure 1
-Sperm head binds to zona pellucida (glycoprotein layer surrounding the oocyte) within 1 day of ovulation in the fallopian tubeacrosome reaction (hydrolytic enzymes released at the head of the sperm)penetrates zona pellucidacell membrane of sperm and egg fuse sperm nucleus and cytoplasm released into eggCompletion of second meiotic division by the secondary oocyte; male & female pronucleus fuse to form zygote
What prevents dispermy (two sperm fertilizing an egg) after entry of the sperm?
1)Depolarization of egg cell membrane prevents other sperm head from binding
2)Egg undergoes cortical reaction: enzymes released by egg hardens the zona pellucida
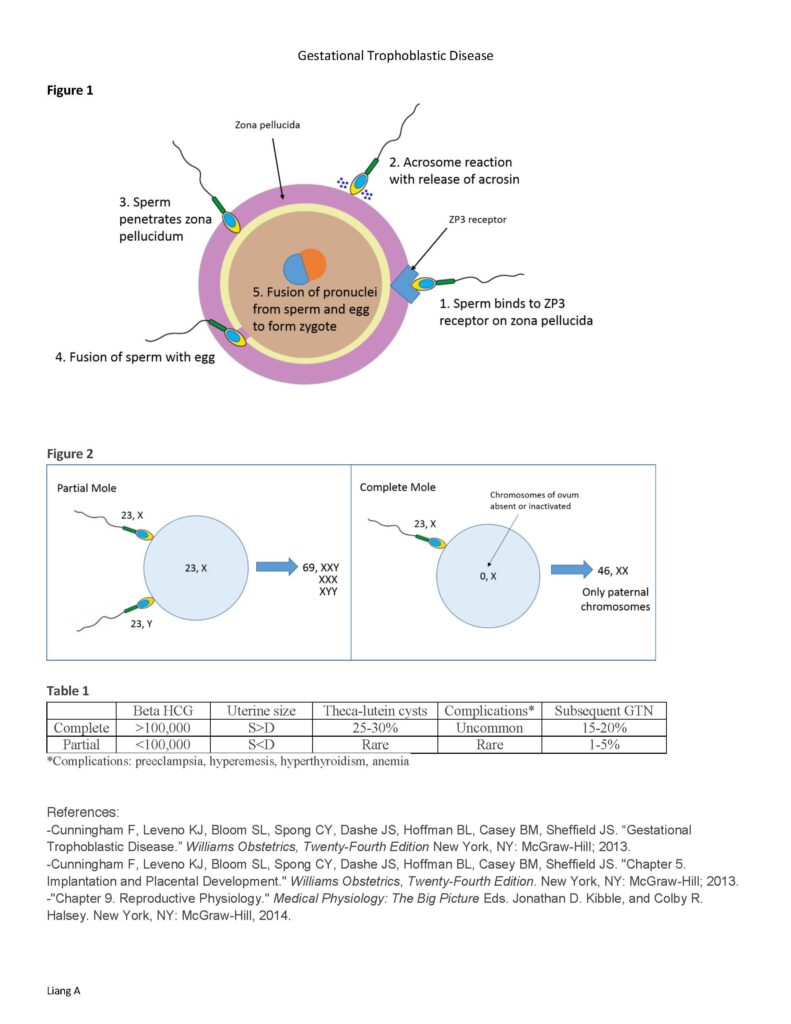
What if the above mechanisms fail? What is the pathogenesis of molar pregnancy?
-Complete: chromosomes of ovum are absent or inactivated; haploid sperm duplicates its own chromosomes after meiosis (androgenesis), both sets of chromosomes are paternal 46 XX
-Partial: 2 paternal haploid sets of chromosomes and 1 maternal haploid set (DISPERMY) triploid 69 XXX, XXY or XYY (more rare)
What is gestational trophoblastic disease? Gestational trophoblastic neoplasm?
Tumors with abnormal trophoblast proliferation; Risks: extremes of age, prior history
1). Hydatiform moles: + villi & edematous immature placenta; Types: complete, partial, invasive
2). Non-molar trophoblastic neoplasms: lack villi; Types: choriocarcinoma, placental site trophoblastic tumor, epithelioid trophoblastic tumor
GTN = subset of GTD with malignant sequelae, includes invasive moles & ALL the non-molar neoplasms
-Develop weeks-years following any type of pregnancy, but > common after complete mole
-Non-metastatic/low risk disease cured with single agent chemotherapy (methotrexate); High risk combination chemotherapy
What are the differences between complete and partial molar pregnancies? See table 1
Complete: edematous villi & abnormal trophoblastic proliferation, NO fetal tissue – grossly appears like clear vesicles; “snowstorm” on ultrasound
Partial: focal and less advanced hydatidiform changes, CONTAINS fetal tissue
What causes hyperthyroid and preeclampsia in molar pregnancy? Rare because of early Dx & Tx
Hyperthyroid: Thyrotropin-like effects of hCG cause ↑T4 and ↓TSH
Preeclampsia: trophoblastic mass releases antiangiogenic factors that activate endothelial damage
How is GTD managed?
–Suction curettage with risk of intraoperative bleeding, particularly with large moles (IV access, blood banking support, uterotonic agents), consider hysterectomy in women >40 ~1/3 will develop GTN
-Serial beta HCG levels (trophoblasts produce hcg)helpful in diagnosis, management & surveillance
-Reliable contraception Gestational Trophoblastic Disease
Liang A
Figure 1
Figure 2
|
Table 1 Beta HCG |
Uterine size |
Theca-lutein cysts |
Complications* |
Subsequent GTN |
|
|
Complete |
>100,000 |
S>D |
25-30% |
Uncommon |
15-20% |
|
Partial |
<100,000 |
S<D |
Rare |
Rare |
1-5% |