Cervical Intraepithelial Neoplasia
Duration 10:14
Cervical Intraepithelial Neoplasia
Liang A
Clinical case applicability: Abnormal pap smear, HPV, genital warts, CIN, cervical cancer
Learning Objectives:
1) Understand the role of HPV in causing cervical intraepithelial neoplasia and cancer
2) Describe the histopathology of cervical intraepithelial neoplasia
What is human papilloma virus (HPV)?
Double-stranded circular DNA virus with 7 early genes E1-E7 (proteins involved in viral gene regulation and cell transformation) & 2 late genes L1-L2 (proteins that form the shell)
What is HPV’s role in CIN? HPV necessary for CIN but HPV alone NOT sufficient to cause CIN. Depends on:
1) Subtype: Determines the oncogenic potential of the virus.
– Low risk types (HPV 6, 11) don’t integrate into host genome (6 & 11 account for 90% of warts)
– High risk types (HPV 16, 18, 31, 33, 35, 39, 45, 51, etc) ↑ persistence & progression to cancer (16 & 18 account for 70% of cervical cancers)
2) Persistence – >50% new HPV infections are cleared in 6-18 months, 80-90% resolve within 2-5 years; Risks for persistence: 1) Older age – 50% persist in women age >55 versus 20% in women <25 (co-testing for screening only in women > 30), 2) High risk subtypes, 3) Duration of infection
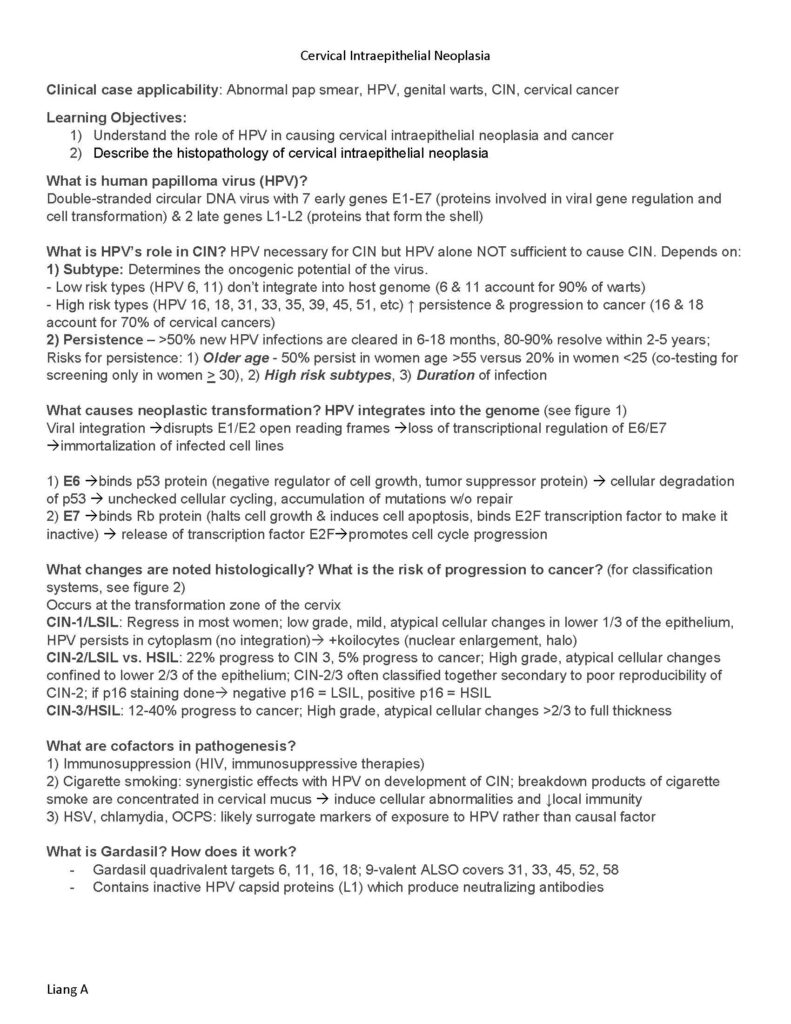
What causes neoplastic transformation? HPV integrates into the genome (see figure 1)
Viral integration disrupts E1/E2 open reading frames loss of transcriptional regulation of E6/E7 immortalization of infected cell lines
1) E6 binds p53 protein (negative regulator of cell growth, tumor suppressor protein) cellular degradation of p53 unchecked cellular cycling, accumulation of mutations w/o repair
2) E7 binds Rb protein (halts cell growth & induces cell apoptosis, binds E2F transcription factor to make it inactive) release of transcription factor E2Fpromotes cell cycle progression
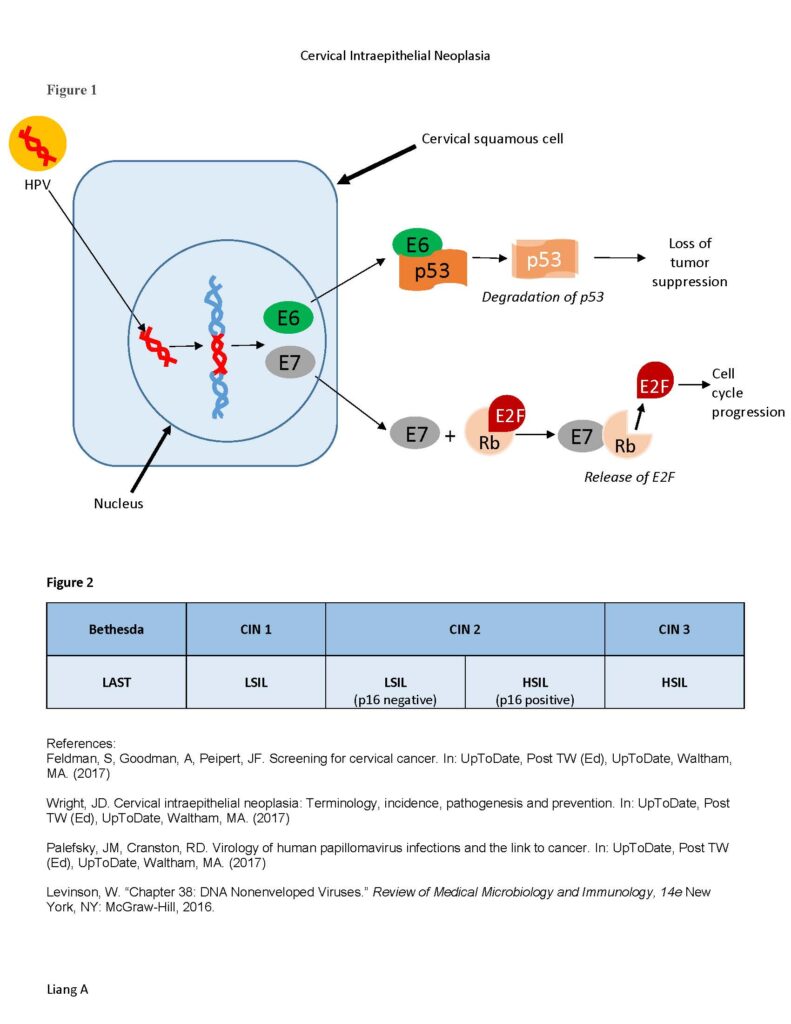
What changes are noted histologically? What is the risk of progression to cancer? (for classification systems, see figure 2)
Occurs at the transformation zone of the cervix
CIN-1/LSIL: Regress in most women; low grade, mild, atypical cellular changes in lower 1/3 of the epithelium, HPV persists in cytoplasm (no integration) +koilocytes (nuclear enlargement, halo)
CIN-2/LSIL vs. HSIL: 22% progress to CIN 3, 5% progress to cancer; High grade, atypical cellular changes confined to lower 2/3 of the epithelium; CIN-2/3 often classified together secondary to poor reproducibility of CIN-2; if p16 staining done negative p16 = LSIL, positive p16 = HSIL
CIN-3/HSIL: 12-40% progress to cancer; High grade, atypical cellular changes >2/3 to full thickness
What are cofactors in pathogenesis?
1) Immunosuppression (HIV, immunosuppressive therapies)
2) Cigarette smoking: synergistic effects with HPV on development of CIN; breakdown products of cigarette smoke are concentrated in cervical mucus induce cellular abnormalities and ↓local immunity
3) HSV, chlamydia, OCPS: likely surrogate markers of exposure to HPV rather than causal factor
What is Gardasil? How does it work?
– Gardasil quadrivalent targets 6, 11, 16, 18; 9-valent ALSO covers 31, 33, 45, 52, 58
– Contains inactive HPV capsid proteins (L1) which produce neutralizing antibodies
Cervical Intraepithelial Neoplasia
Liang A
HPV
E6
E7
E6
p53
Degradation of p53
Loss of
tumor
suppression
Cervical squamous cell
Nucleus
E7
Rb
E2F
Cell
cycle
progression
E7
Rb
E2F
+
Release of E2F
Figure 1
p53
|
Figure 2 Bethesda |
CIN 1 |
CIN 2 |
CIN 3 |
|
|
LAST |
LSIL |
LSIL (p16 negative) |
HSIL (p16 positive) |
HSIL |