Contraception
Duration 9:54
Teaching Script: Contraception
Clinical Case Applicability:
Patient desires contraception, Conception contraindicated in patient with comorbid condition
Learning Objectives:
1) To review the different forms of contraception available to prevent pregnancy
2) To understand the mechanism of action for each form of contraception
3) To understand contraindications to each option as well as other clinical considerations for use
Clinical Presentation:
Patient with history of lupus and severe preeclampsia in first pregnancy; declines tubal ligation but accepts non-permanent
contraception.
What types of contraception are available to prevent pregnancy?
• Hormonal options
o Estrogen/Progesterone (E/P) options: Oral contraceptive pills (OCP), patch, ring
o Progesterone only: pills, implant, injectable and levonorgesterel intrauterine device (IUD)
• Non Hormonal options
o Lactational amenorrhea
o Fertility awareness: calendar method, cervical mucous, symptothermal
o Barrier methods: condoms, diaphragm/cap, spermicide
What are the necessary steps for conception that must be prevented?
1. Sperm deposited in vagina
2. Sperm passes through cervix and uterus to reach fallopian tube
3. Ovulation occurs and oocyte is released into fallopian tube
4. Sperm and oocyte meet in fallopian tube and fertilization occurs
5. Blastocyst implants in endometrium
• Three main mechanisms of birth control prevent ovulation, prevent fertilization, prevent implantation
Which methods will prevent ovulation?
• Methods focused on ovulation prevention: OCP, Depoprovera, Progestin IUD, Etonogestrel implant, Lactational amenorrhea
• Exogenous progestin (and estrogen) lead to suppression of gonadotropin-releasing hormone (GnRH) release form hypothalamus
which decreases luteinizing hormone (LH) and follicle stimulating hormone (FSH) from the pituitary and thus blocks ovarian
follicular development
• Lactational amenorrhea: infant suckling interrupts pulsatile GnRH secretion leading to decrease in LH/FSH and anovulation –
elevated prolactin appears to inhibit LH, via inhibition of the release of GnRH.
Which methods prevent fertilization?
• Physical Barriers
o Condoms
§ Male: Protects against many STI
§ Female: polyurethane sheath with polyurethane ring, protects again HIV, CMV and HepB
o Diaphragm: rubber dome with silicone membrane, apply water based spermicide; must use every time; some STI
prevention
o Permanent Sterilization
§ Vasectomy: interrupts vas deferens between testes and penis
§ Female tubal surgery interrupts fallopian tubes –open procedure, laparoscopy, occlude with clips/bands or
hysteroscopy with Essure
o Thicken cervical mucous (progesterone only pills, implants, progestin IUD),
§ Maintains thick/scant or impenetrable to sperm
• Chemical Barriers
o Spermicides and microbicides
§ Cream jellies, suppositories, film and foam
§ Physical and chemical barrier with nonoxynol-9 or octoxynol-9
o Copper IUD
§ T-shaped polyethylene with barium sulfate and total of 380mm2 of copper
§ Interferes with sperm motility and local inflammation that is toxic to sperm and egg
• Temporal Barriers
o Fertility awareness based methods, withdrawal, Abstinence
§ Advantage: cheap, readily available (apps and web), compatible with religious teachings
§ Disadvantage: require proper knowledge for use, need a regular menstrual cycle, need cooperation from both
partners – must be consistent
o Emergency contraception: will not disrupt established pregnancy
§ Levonorgestral most effective 72 hours after sex to delay ovulation
§ Ulipristal acetate – approved for use up to 5 days after intercourse
§ Prescription only, selective progestin receptor modulator – binds but does not activate progesterone receptor,
interferes with dominant follicle recruitment and block ovulation even after LH surge
Which methods prevent implantation?
• IUDS (hormonal and non hormonal) create inflammation that is unfavorable to implantation
• Progestins thin out endometrium so it is unfavorable; endometrium stays in resting state
• Specifically MIUD creates a constant resting state endometrium that decreases bleeding by >50% and 20% amenorrhea
How does the pharmacology of E/P vs P only methods differ in preventing conception?
• Progestin: dominant component, suppresses LH secretion and the LH surge through negative feedback on pituitary and
hypothalamus to inhibit ovulation
o In addition, leads to thickened cervical mucous, thin inactive endometrium, some will decrease ovarian hormone
production, may interfere with egg transport via tubal peristalsis and with spermatic enzyme activity
• Estrogen: suppresses FSH and prevents follicle recruitment, maturation and ovulation via negative feedback. It also increases
progesterone effect by potentiating the concentration of progesterone receptors. Counters P atrophic effects on endometrium
via proliferation to decrease irregular bleeding
• Hormone composition
o Estrogens are either: Ethinyl Estradiol (EE) or Estradiol Valerate (EV)
o Progestin component:
§ Testosterone derived (most common) Norethindrone, or Gonanes (levo-norgesterel, norgestimate,
desogestrel, etonogesterel)
§ Spironolactone analog – drospirenone
§ Progesterone analog: medroxyprogesterone acetate
What Contraindications to hormonal contraception use should be considered?
a. Estrogen: migraine with aura, CV disease, personal history of VTE, immediate post partum period, stroke, age >35 and
smoker, severe HTN, DM with vascular complication and known thrombogenic mutation (category 3-4 conditions) –
mostly due to the pro thrombotic nature of estrogen
b. Progesterone: personal history of breast cancer, severe decompensated cirrhosis, gestational trophoblastic disease,
hepatocellular adenoma and lupus with positive antiphospholipid antibodies
References:
• Beckmann, CRB, et al. Obstetrics and Gynecology. 8th edition. Baltimore, MD: Lippincott, Williams, and Wilkins, 2018.
• Hoffman, BL, et al. William’s Gynecology. 3rd edition. McGraw-Hill Education. 2016.
• https://www.cdc.gov/reproductivehealth/unintendedpregnancy/pdf/legal_summary-chart_english_final_tag508.pdf
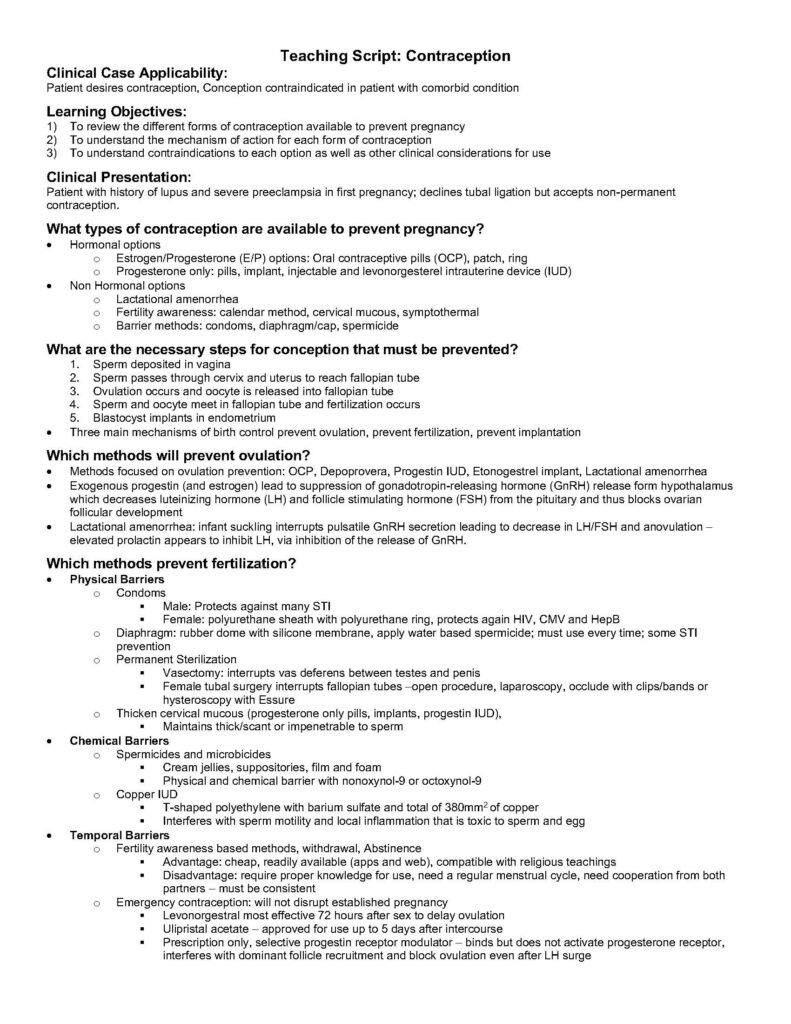
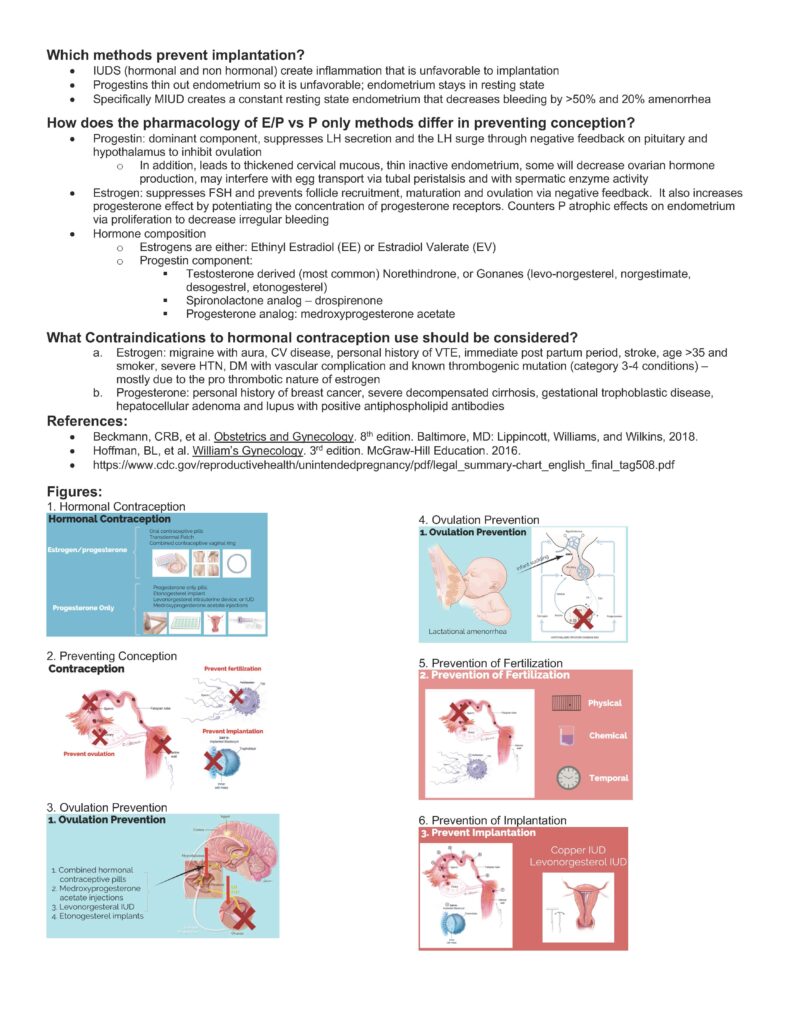
Figures:
1. Hormonal Contraception
2. Preventing Conception
3. Ovulation Prevention
4. Ovulation Prevention
5. Prevention of Fertilization
6. Prevention of Implantation