Dysmenorrhea
Duration 10:13
Dysmenorrhea
Plummer XD, Liang A
Clinical Cases Applicability: dysmenorrhea, pelvic pain, endometriosis, adenomyosis
Learning Objectives:
1. Understand the histology of the normal endometrium and myometrium
2. Understand the pathophysiology behind dysmenorrhea and endometriosis
3. Understand the pharmacological treatment of dysmenorrhea
What are the normal histology and function of the endometrium and myometrium?
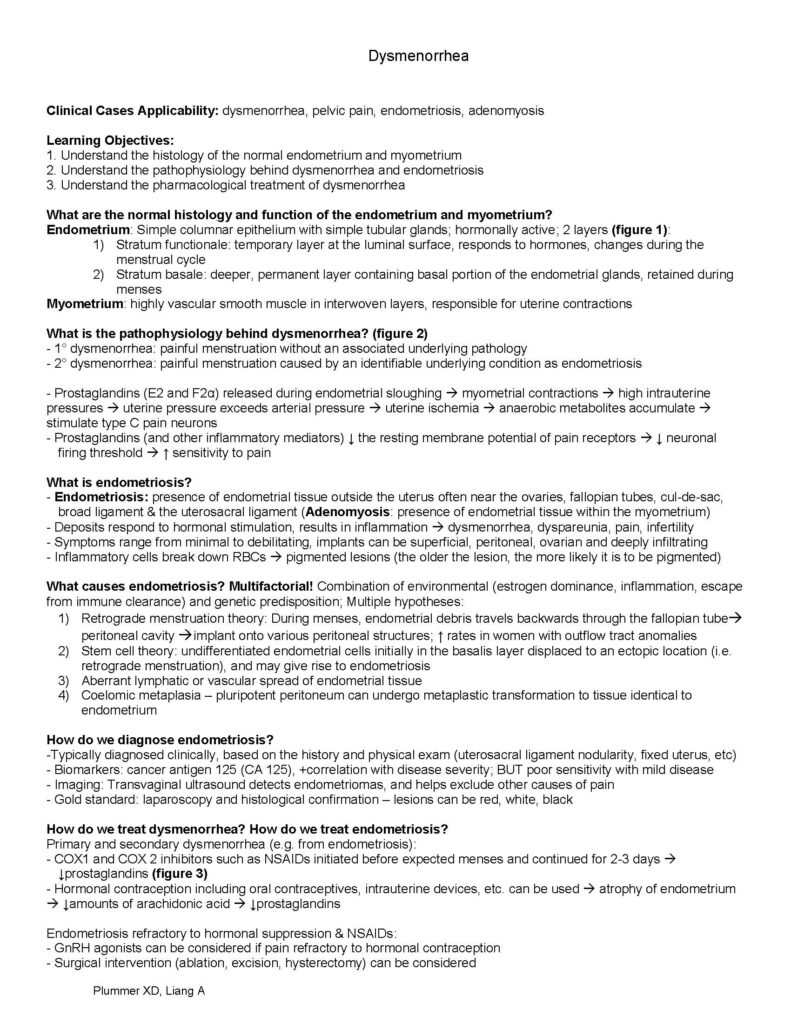
Endometrium: Simple columnar epithelium with simple tubular glands; hormonally active; 2 layers (figure 1):
1) Stratum functionale: temporary layer at the luminal surface, responds to hormones, changes during the menstrual cycle
2) Stratum basale: deeper, permanent layer containing basal portion of the endometrial glands, retained during menses
Myometrium: highly vascular smooth muscle in interwoven layers, responsible for uterine contractions
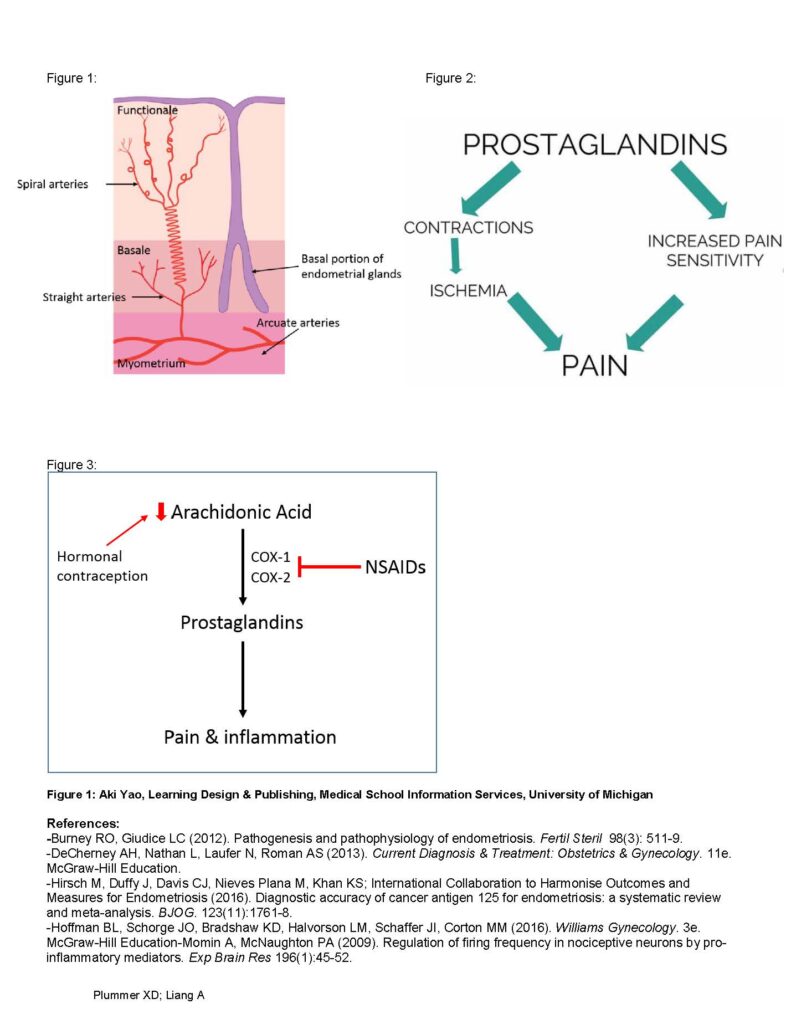
What is the pathophysiology behind dysmenorrhea? (figure 2)
– 1° dysmenorrhea: painful menstruation without an associated underlying pathology
– 2° dysmenorrhea: painful menstruation caused by an identifiable underlying condition as endometriosis
– Prostaglandins (E2 and F2α) released during endometrial sloughing myometrial contractions high intrauterine pressures uterine pressure exceeds arterial pressure uterine ischemia anaerobic metabolites accumulate stimulate type C pain neurons
– Prostaglandins (and other inflammatory mediators) ↓ the resting membrane potential of pain receptors ↓ neuronal firing threshold ↑ sensitivity to pain
What is endometriosis?
– Endometriosis: presence of endometrial tissue outside the uterus often near the ovaries, fallopian tubes, cul-de-sac, broad ligament & the uterosacral ligament (Adenomyosis: presence of endometrial tissue within the myometrium)
– Deposits respond to hormonal stimulation, results in inflammation dysmenorrhea, dyspareunia, pain, infertility
– Symptoms range from minimal to debilitating, implants can be superficial, peritoneal, ovarian and deeply infiltrating
– Inflammatory cells break down RBCs pigmented lesions (the older the lesion, the more likely it is to be pigmented)
What causes endometriosis? Multifactorial! Combination of environmental (estrogen dominance, inflammation, escape from immune clearance) and genetic predisposition; Multiple hypotheses:
1) Retrograde menstruation theory: During menses, endometrial debris travels backwards through the fallopian tube peritoneal cavity implant onto various peritoneal structures; ↑ rates in women with outflow tract anomalies
2) Stem cell theory: undifferentiated endometrial cells initially in the basalis layer displaced to an ectopic location (i.e. retrograde menstruation), and may give rise to endometriosis
3) Aberrant lymphatic or vascular spread of endometrial tissue
4) Coelomic metaplasia – pluripotent peritoneum can undergo metaplastic transformation to tissue identical to endometrium
How do we diagnose endometriosis?
-Typically diagnosed clinically, based on the history and physical exam (uterosacral ligament nodularity, fixed uterus, etc)
– Biomarkers: cancer antigen 125 (CA 125), +correlation with disease severity; BUT poor sensitivity with mild disease
– Imaging: Transvaginal ultrasound detects endometriomas, and helps exclude other causes of pain
– Gold standard: laparoscopy and histological confirmation – lesions can be red, white, black
How do we treat dysmenorrhea? How do we treat endometriosis?
Primary and secondary dysmenorrhea (e.g. from endometriosis):
– COX1 and COX 2 inhibitors such as NSAIDs initiated before expected menses and continued for 2-3 days ↓prostaglandins (figure 3)
– Hormonal contraception including oral contraceptives, intrauterine devices, etc. can be used atrophy of endometrium ↓amounts of arachidonic acid ↓prostaglandins
Endometriosis refractory to hormonal suppression & NSAIDs:
– GnRH agonists can be considered if pain refractory to hormonal contraception
– Surgical intervention (ablation, excision, hysterectomy) can be considered Plummer XD; Liang A
Figure 1: Figure 2:
Figure 3:
Figure 1: Aki Yao, Learning Design & Publishing, Medical School Information Services, University of Michigan
References:
–Burney RO, Giudice LC (2012). Pathogenesis and pathophysiology of endometriosis. Fertil Steril 98(3): 511-9.
-DeCherney AH, Nathan L, Laufer N, Roman AS (2013). Current Diagnosis & Treatment: Obstetrics & Gynecology. 11e. McGraw-Hill Education.
-Hirsch M, Duffy J, Davis CJ, Nieves Plana M, Khan KS; International Collaboration to Harmonise Outcomes and Measures for Endometriosis (2016). Diagnostic accuracy of cancer antigen 125 for endometriosis: a systematic review and meta-analysis. BJOG. 123(11):1761-8.
-Hoffman BL, Schorge JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM (2016). Williams Gynecology. 3e. McGraw-Hill Education-Momin A, McNaughton PA (2009). Regulation of firing frequency in nociceptive neurons by pro-inflammatory mediators. Exp Brain Res 196(1):45-52.