Hemorrhage
Duration 9:41
Liang A
Disseminated Intravascular Coagulation (DIC)
Clinical Cases Applicability: Postpartum hemorrhage, HELLP Syndrome, Placental abruption, Fetal demise, Amniotic fluid embolism
Learning Objectives:
1) Understand the basic principles of normal hemostasis
2) Understand which clotting factors are measured in commonly ordered coagulation labs 3) Understand the pathophysiology of DIC
Clinical Presentation: Bleeding, hypotension out of proportion to bleeding, and coagulopathy
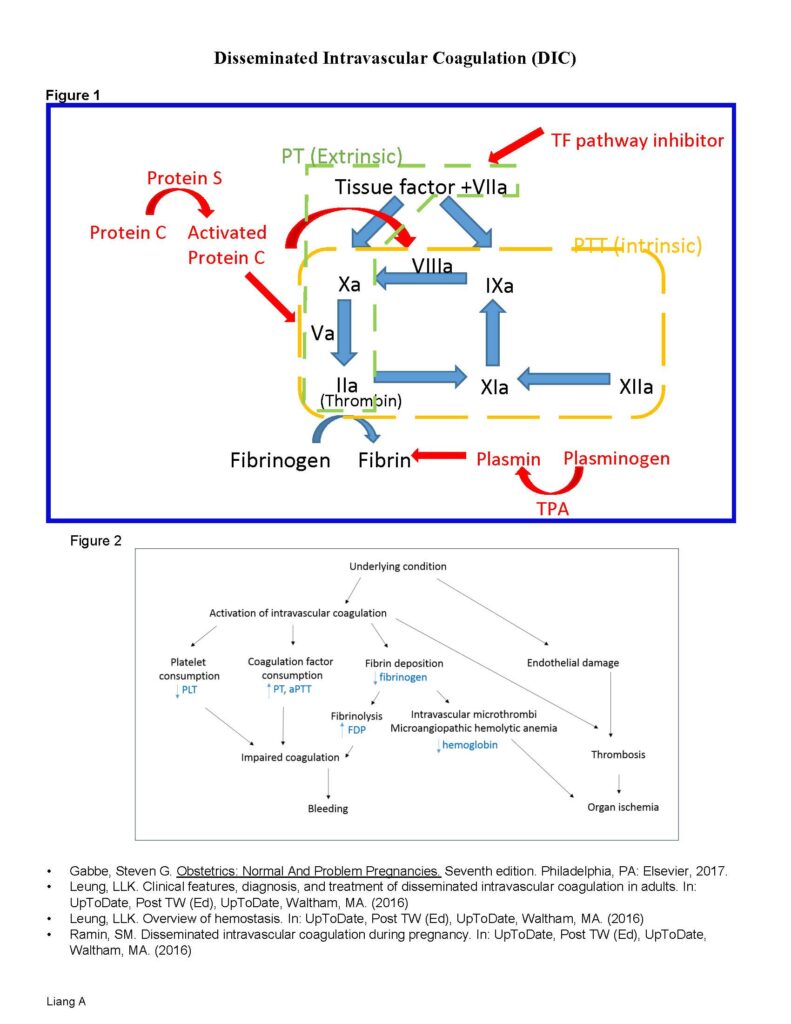
How does a clot form? (See figure 1)
Tissue factor at the wound site + VIIa activates X and IX to generate small amounts of thrombin activates factors V, VIII, XI and platelets, which leads to amplification of thrombin How does a clot stop forming?
1)Antithrombin inhibits thrombin 2)Activated protein C block activation of factors V and VIII 3)Tissue factor pathway inhibitor blocks activation of factor VII
How is a clot removed (fibrinolytic system)?
Fibrin & tissue plasminogen activator bind plasminogen plasmin cleaves fibrin releases FDP (fibrin degradation products)
What clotting factors are measured when you order aPTT? PT?
-aPTT: “Intrinsic” pathway; all coagulation factors except VII and tissue factor
-PT: “Extrinsic” pathway; tissue factor, VII, V, X, II (prothrombin), fibrinogen
-factor VII, IX, X, II, protein C&S are vitamin K dependent altered by warfarin
What happens in DIC? See figure 2
Coagulation and fibrinolysis become abnormally activated within the vasculature
Endothelial damage activation of coagulation cascade extensive thrombi in microvasculature and larger vesselsconsumption of factors, platelets and anticoagulant factors (S, C, antithrombin) consumption greater than production “consumptive coagulopathy”fibrinolysislarge amount of FDP interferes with fibrin clot formation and platelet aggregationtissue/organ damage from reduced perfusion, thrombosis and/or bleeding
Pathophysiology in pregnancy:
Decidual cells lining the vascular bed of the placenta strongly express tissue factor (similar to endothelial cells);
TF released at sites of decidual traumacoagulation cascade activation
-Abruption, fetal demise: Release of procoagulants due to significant injury/necrosis of fetoplacental tissue
-AFE: Amniotic fluid rich in procoagulants and anticoagulants
-Preeclampsia, HELLP: Contribute to endothelial cell damage
-Hemorrhage leading to shock: severe tissue hypoxia proposed to result in release of TF from damaged cells
What are laboratory findings that are consistent with DIC?
↓Platelets, hemolytic changes in peripheral blood smear (anemia & schistocytes), ↓fibrinogen (normal fibrinogen levels range from 373 -619 mg/dL in 3rd trimester), ↑D-dimer (FDP), and ↑ PT and aPTT.
How do you treat DIC?
Focused on correcting the underlying cause, maintenance of maternal volume status, and replacement of blood products: platelets, fresh frozen plasma (contains all coagulation factors), cryoprecipitate (smaller volume than FFP, rich in von Willebrand factor, VIII, XIII, fibrinogen) Liang A
Figure 2
Tissue factor +VIIa
Xa
IXa
VIIIa
Va
IIa
(
Thrombin
)
XIa
XIIa
Fibrinogen
Fibrin
Plasmin
Plasminogen
TPA
TF pathway inhibitor
Protein C
Activated
Protein C
Protein S
PTT (intrinsic)
PT (Extrinsic)
Disseminated Intravascular Coagulation (DIC)
Figure 1
• Gabbe, Steven G. Obstetrics: Normal And Problem Pregnancies. Seventh edition. Philadelphia, PA: Elsevier, 2017.
• Leung, LLK. Clinical features, diagnosis, and treatment of disseminated intravascular coagulation in adults. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2016)
• Leung, LLK. Overview of hemostasis. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2016)
• Ramin, SM. Disseminated intravascular coagulation during pregnancy. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2016)