Hirsutism
Duration 13:47
Teaching Script: Hirsutism
Clinical Case Applicability:
Hirsutism, Polycystic Ovarian Syndrome, Androgen-secreting Ovarian Tumors
Learning Objectives:
1) Review the clinical definition, etiology, and diagnostic criteria for hirsutism in the APGO Clinical Video Topic 44
2) Identify where are androgens produced in women and the role of androgens in development of hirsutism.
3) Compare and contrast the normal pathway of ovarian steroidogenesis, particularly androgens, with the pathologic mechanisms
leading to abnormal androgen secretion
4) Describe the mechanism of action and potential side effects of medications commonly used to treat hirsutism.
Clinical Presentation:
22 year old women with moderate obesity, unwanted facial and chest hair, and oligomenorrhea
What is the etiology of hirsutism in women and how is it diagnosed?
• Review APGO Clinical Video Topic 44
• 5-10% reproductive age women have hirsutism, defined as excess male pattern hair growth
• Most common cause is Polycystic Ovarian Syndrome (PCOS)
• Etiologies include: Familial, Idiopathic, PCOS, Ovarian (most frequent androgen-secreting tumor) or Adrenal Tumor,
Pharmacologic agents (ex. danazol, testosterone, dehydroepiandrosterone sulfate (DHEAS), corticosteroids, diazoxide)
o Rapidly progressing signs of androgen excess should prompt evaluation for androgen-secreting neoplasm (ovarian –
testosterone >200ng/dL; or adrenal – DHEAS twice normal) or Cushing syndrome
• Laboratory testing: bioavailable or calculated free T level, DHEAS, 17-hydroxyprogesterone; Add LH, FSH, Prolactin and TSH if
associated oligo- or amenorrhea. 24-hour urinary cortisol or dexamethasone suppression test if Cushing syndrome suspected.
• Important to check free testosterone (T) in mild to moderate hirsutism as total T may be normal.
• About 75% testosterone bound to sex-hormone binding globulin (SHBG), ~20% bound to albumin and small % unbound.
• Level of bioavailable testosterone related to albumin: T ratio, total albumin, total T, and SHBG
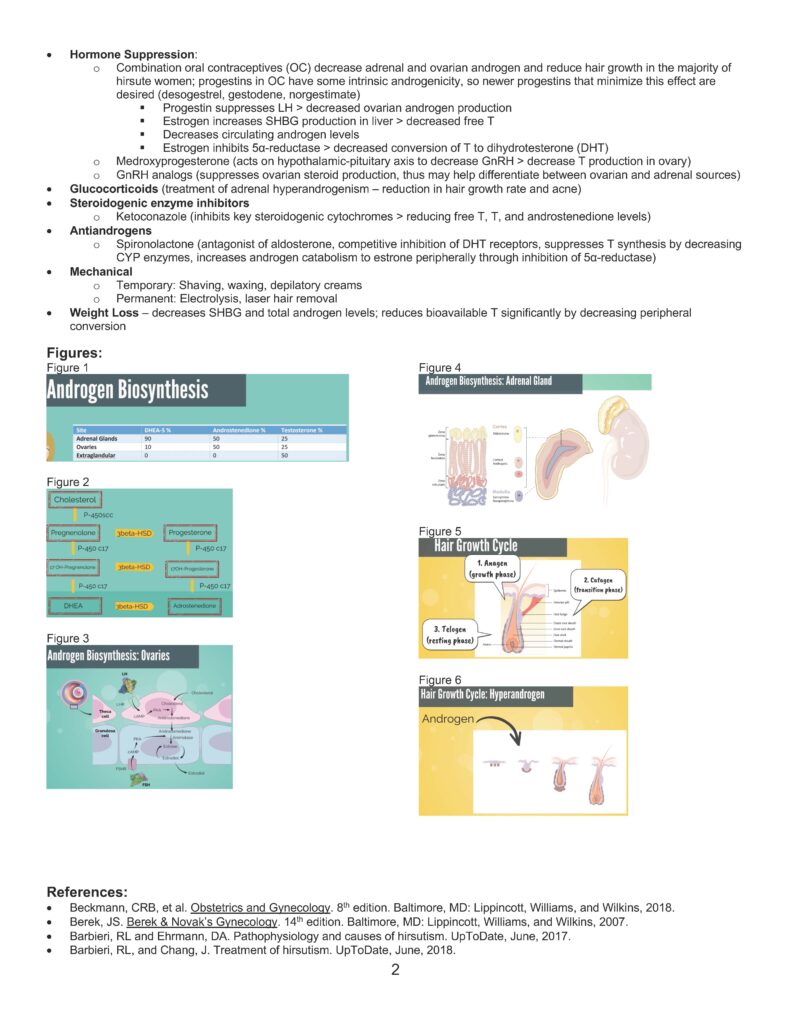
How do androgens affect hair growth?
• Hair growth cycle: 1) Anagen or growth phase (~6 months); 2) Catagen or involutional phase (2-3 weeks); 3) Telogen or resting
phase (2-3 weeks) with mature root sheath or clubbed proximal end
o Excess androgens increase the anagen phase, and result in predominantly terminal hair (long, course, pigmented) rather
than vellus hair (fine, soft)
• Androgens increase distribution in sensitive areas: upper lip, chin, midsternum, upper abdomen, back and buttocks
• Androgens decrease distribution on scalp with a reduced anagen phase.
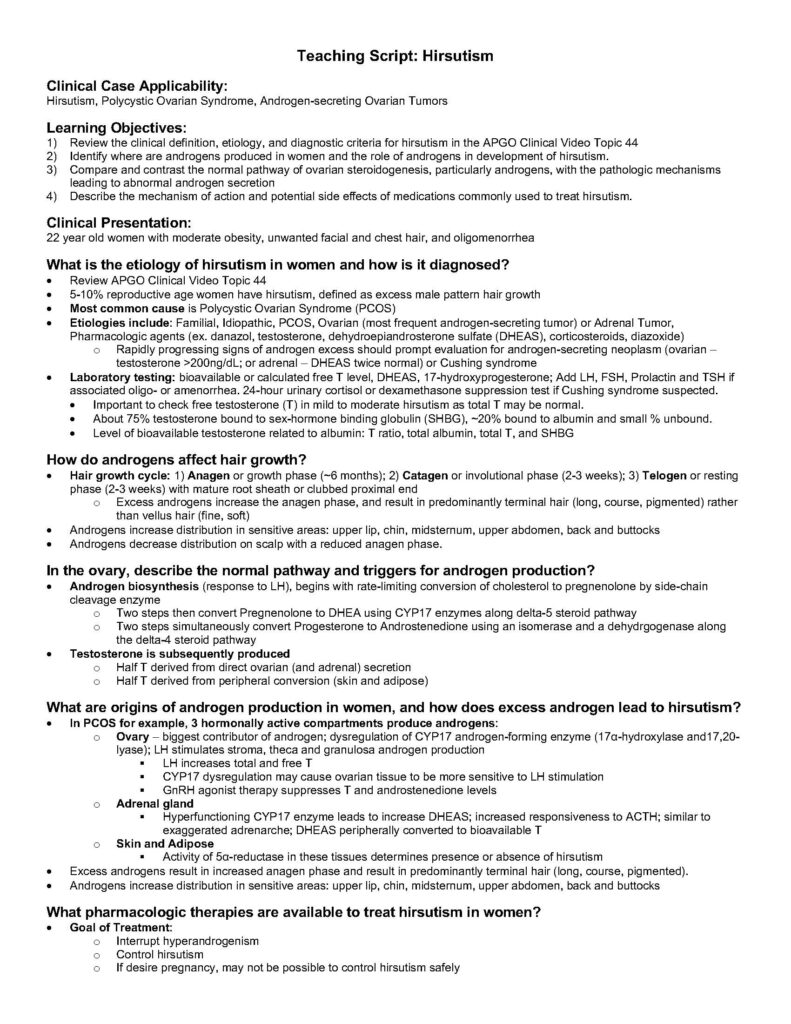
In the ovary, describe the normal pathway and triggers for androgen production?
• Androgen biosynthesis (response to LH), begins with rate-limiting conversion of cholesterol to pregnenolone by side-chain
cleavage enzyme
o Two steps then convert Pregnenolone to DHEA using CYP17 enzymes along delta-5 steroid pathway
o Two steps simultaneously convert Progesterone to Androstenedione using an isomerase and a dehydrgogenase along
the delta-4 steroid pathway
• Testosterone is subsequently produced
o Half T derived from direct ovarian (and adrenal) secretion
o Half T derived from peripheral conversion (skin and adipose)
What are origins of androgen production in women, and how does excess androgen lead to hirsutism?
• In PCOS for example, 3 hormonally active compartments produce androgens:
o Ovary – biggest contributor of androgen; dysregulation of CYP17 androgen-forming enzyme (17α-hydroxylase and17,20-
lyase); LH stimulates stroma, theca and granulosa androgen production
§ LH increases total and free T
§ CYP17 dysregulation may cause ovarian tissue to be more sensitive to LH stimulation
§ GnRH agonist therapy suppresses T and androstenedione levels
o Adrenal gland
§ Hyperfunctioning CYP17 enzyme leads to increase DHEAS; increased responsiveness to ACTH; similar to
exaggerated adrenarche; DHEAS peripherally converted to bioavailable T
o Skin and Adipose
§ Activity of 5α-reductase in these tissues determines presence or absence of hirsutism
• Excess androgens result in increased anagen phase and result in predominantly terminal hair (long, course, pigmented).
• Androgens increase distribution in sensitive areas: upper lip, chin, midsternum, upper abdomen, back and buttocks
What pharmacologic therapies are available to treat hirsutism in women?
• Goal of Treatment:
o Interrupt hyperandrogenism
o Control hirsutism
o If desire pregnancy, may not be possible to control hirsutism safely
2
• Hormone Suppression:
o Combination oral contraceptives (OC) decrease adrenal and ovarian androgen and reduce hair growth in the majority of
hirsute women; progestins in OC have some intrinsic androgenicity, so newer progestins that minimize this effect are
desired (desogestrel, gestodene, norgestimate)
§ Progestin suppresses LH > decreased ovarian androgen production
§ Estrogen increases SHBG production in liver > decreased free T
§ Decreases circulating androgen levels
§ Estrogen inhibits 5α-reductase > decreased conversion of T to dihydrotesterone (DHT)
o Medroxyprogesterone (acts on hypothalamic-pituitary axis to decrease GnRH > decrease T production in ovary)
o GnRH analogs (suppresses ovarian steroid production, thus may help differentiate between ovarian and adrenal sources)
• Glucocorticoids (treatment of adrenal hyperandrogenism – reduction in hair growth rate and acne)
• Steroidogenic enzyme inhibitors
o Ketoconazole (inhibits key steroidogenic cytochromes > reducing free T, T, and androstenedione levels)
• Antiandrogens
o Spironolactone (antagonist of aldosterone, competitive inhibition of DHT receptors, suppresses T synthesis by decreasing
CYP enzymes, increases androgen catabolism to estrone peripherally through inhibition of 5α-reductase)
• Mechanical
o Temporary: Shaving, waxing, depilatory creams
o Permanent: Electrolysis, laser hair removal
• Weight Loss – decreases SHBG and total androgen levels; reduces bioavailable T significantly by decreasing peripheral
conversion
Figures:
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
References:
• Beckmann, CRB, et al. Obstetrics and Gynecology. 8th edition. Baltimore, MD: Lippincott, Williams, and Wilkins, 2018.
• Berek, JS. Berek & Novak’s Gynecology. 14th edition. Baltimore, MD: Lippincott, Williams, and Wilkins, 2007.
• Barbieri, RL and Ehrmann, DA. Pathophysiology and causes of hirsutism. UpToDate, June, 2017.
• Barbieri, RL, and Chang, J. Treatment of hirsutism. UpToDate, June, 2018.