Hypertensive Disease of Pregnancy
Duration 10:39
Hypertensive Disease in Pregnancy
Clinical Cases Applicability: Chronic Hypertension, Preeclampsia (PreE), Eclampsia, HELLP, AFLP
Learning Objectives:
• Describe the physiology of normal regulation of blood pressure in pregnancy
• Understand proposed pathophysiology of preeclampsia and associated end organ damage
• Compare and contrast the pharmacology of anti-hypertensive medications used in pregnancy
• Describe the mechanism of action of magnesium in the prevention of recurrent eclamptic seizures
Clinical Presentation: Patient with chronic hypertension develops worsening hypertension in the third trimester; a
nulliparous patient has an eclamptic seizure in the third trimester; a laboring patient presents with new onset hypertension
and proteinuria
Review the spectrum of hypertensive diseases in pregnancy (Review the corresponding videos for
APGO Medical Student Educational Topics 8 and 18)
• Preeclampsia-eclampsia
• Chronic hypertension
• Chronic hypertension with superimposed preeclampsia
• Gestational hypertension
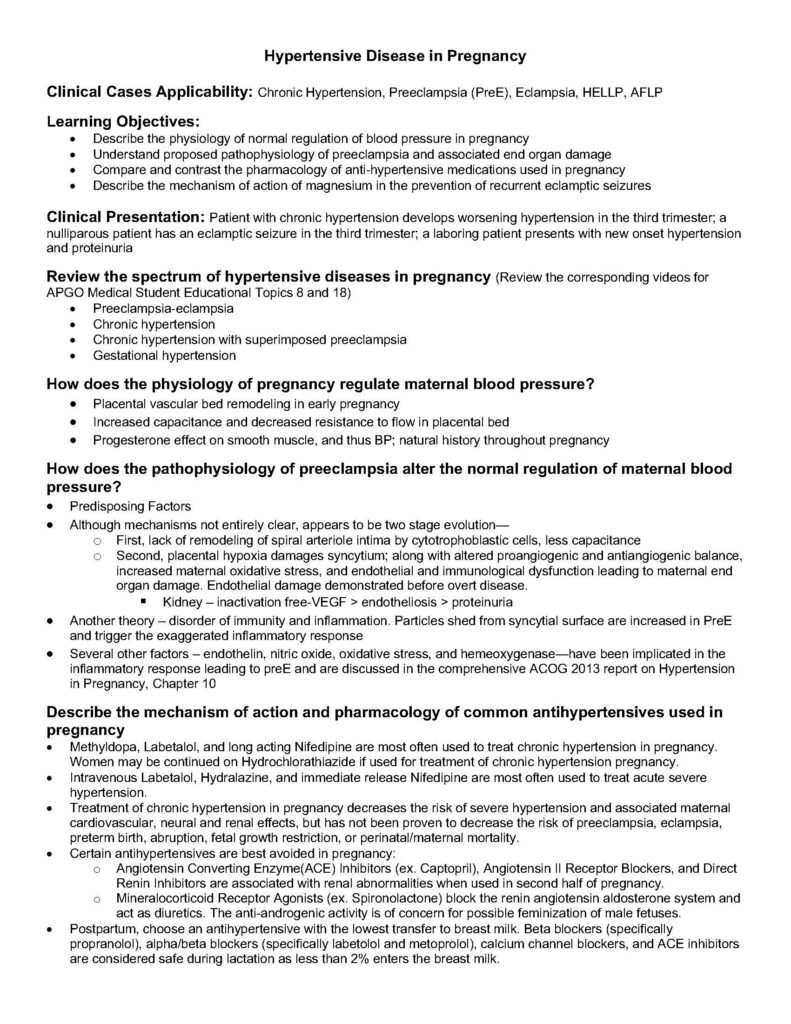
How does the physiology of pregnancy regulate maternal blood pressure?
• Placental vascular bed remodeling in early pregnancy
• Increased capacitance and decreased resistance to flow in placental bed
• Progesterone effect on smooth muscle, and thus BP; natural history throughout pregnancy
How does the pathophysiology of preeclampsia alter the normal regulation of maternal blood
pressure?
• Predisposing Factors
• Although mechanisms not entirely clear, appears to be two stage evolution—
o First, lack of remodeling of spiral arteriole intima by cytotrophoblastic cells, less capacitance
o Second, placental hypoxia damages syncytium; along with altered proangiogenic and antiangiogenic balance,
increased maternal oxidative stress, and endothelial and immunological dysfunction leading to maternal end
organ damage. Endothelial damage demonstrated before overt disease.
§ Kidney – inactivation free-VEGF > endotheliosis > proteinuria
• Another theory – disorder of immunity and inflammation. Particles shed from syncytial surface are increased in PreE
and trigger the exaggerated inflammatory response
• Several other factors – endothelin, nitric oxide, oxidative stress, and hemeoxygenase—have been implicated in the
inflammatory response leading to preE and are discussed in the comprehensive ACOG 2013 report on Hypertension
in Pregnancy, Chapter 10
Describe the mechanism of action and pharmacology of common antihypertensives used in
pregnancy
• Methyldopa, Labetalol, and long acting Nifedipine are most often used to treat chronic hypertension in pregnancy.
Women may be continued on Hydrochlorathiazide if used for treatment of chronic hypertension pregnancy.
• Intravenous Labetalol, Hydralazine, and immediate release Nifedipine are most often used to treat acute severe
hypertension.
• Treatment of chronic hypertension in pregnancy decreases the risk of severe hypertension and associated maternal
cardiovascular, neural and renal effects, but has not been proven to decrease the risk of preeclampsia, eclampsia,
preterm birth, abruption, fetal growth restriction, or perinatal/maternal mortality.
• Certain antihypertensives are best avoided in pregnancy:
o Angiotensin Converting Enzyme(ACE) Inhibitors (ex. Captopril), Angiotensin II Receptor Blockers, and Direct
Renin Inhibitors are associated with renal abnormalities when used in second half of pregnancy.
o Mineralocorticoid Receptor Agonists (ex. Spironolactone) block the renin angiotensin aldosterone system and
act as diuretics. The anti-androgenic activity is of concern for possible feminization of male fetuses.
• Postpartum, choose an antihypertensive with the lowest transfer to breast milk. Beta blockers (specifically
propranolol), alpha/beta blockers (specifically labetolol and metoprolol), calcium channel blockers, and ACE inhibitors
are considered safe during lactation as less than 2% enters the breast milk.
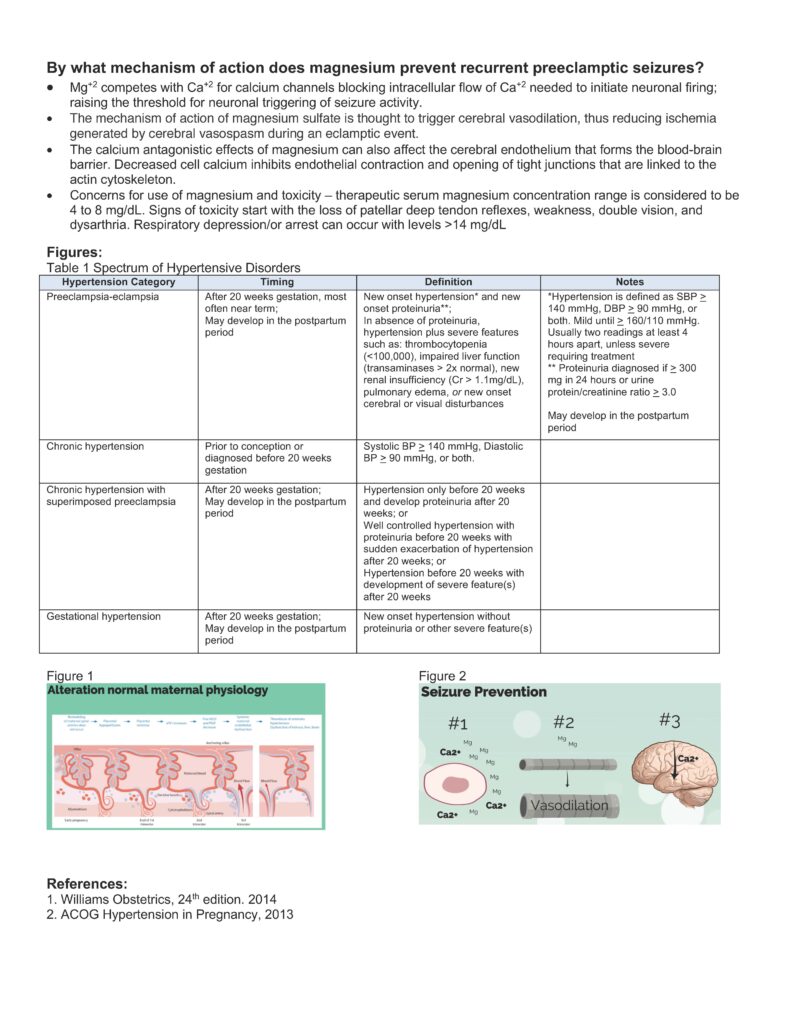
By what mechanism of action does magnesium prevent recurrent preeclamptic seizures?
• Mg+2 competes with Ca+2 for calcium channels blocking intracellular flow of Ca+2 needed to initiate neuronal firing;
raising the threshold for neuronal triggering of seizure activity.
• The mechanism of action of magnesium sulfate is thought to trigger cerebral vasodilation, thus reducing ischemia
generated by cerebral vasospasm during an eclamptic event.
• The calcium antagonistic effects of magnesium can also affect the cerebral endothelium that forms the blood-brain
barrier. Decreased cell calcium inhibits endothelial contraction and opening of tight junctions that are linked to the
actin cytoskeleton.
• Concerns for use of magnesium and toxicity – therapeutic serum magnesium concentration range is considered to be
4 to 8 mg/dL. Signs of toxicity start with the loss of patellar deep tendon reflexes, weakness, double vision, and
dysarthria. Respiratory depression/or arrest can occur with levels >14 mg/dL
Figures:
Table 1 Spectrum of Hypertensive Disorders
Hypertension Category Timing Definition Notes
Preeclampsia-eclampsia After 20 weeks gestation, most
often near term;
May develop in the postpartum
period
New onset hypertension* and new
onset proteinuria**;
In absence of proteinuria,
hypertension plus severe features
such as: thrombocytopenia
(<100,000), impaired liver function
(transaminases > 2x normal), new
renal insufficiency (Cr > 1.1mg/dL),
pulmonary edema, or new onset
cerebral or visual disturbances
*Hypertension is defined as SBP >
140 mmHg, DBP > 90 mmHg, or
both. Mild until > 160/110 mmHg.
Usually two readings at least 4
hours apart, unless severe
requiring treatment
** Proteinuria diagnosed if > 300
mg in 24 hours or urine
protein/creatinine ratio > 3.0
May develop in the postpartum
period
Chronic hypertension Prior to conception or
diagnosed before 20 weeks
gestation
Systolic BP > 140 mmHg, Diastolic
BP > 90 mmHg, or both.
Chronic hypertension with
superimposed preeclampsia
After 20 weeks gestation;
May develop in the postpartum
period
Hypertension only before 20 weeks
and develop proteinuria after 20
weeks; or
Well controlled hypertension with
proteinuria before 20 weeks with
sudden exacerbation of hypertension
after 20 weeks; or
Hypertension before 20 weeks with
development of severe feature(s)
after 20 weeks
Gestational hypertension After 20 weeks gestation;
May develop in the postpartum
period
New onset hypertension without
proteinuria or other severe feature(s)
Figure 1
Figure 2
References:
1. Williams Obstetrics, 24th edition. 2014
2. ACOG Hypertension in Pregnancy, 2013