Menopause
Duration 10:04
Menopause
Liang A
Clinical Cases Applicability: menopausal symptoms (hot flashes, atrophy), osteopenia/osteoporosis, menopausal hormone, premature ovarian insufficiency
Learning Objectives:
1. Understand the physiologic changes in estrogen levels and the hypothalamic-pituitary-ovarian axis in menopause
2. Describe the pathophysiology of the various symptoms of peri-menopause/menopause
3. Discuss treatment options for the symptoms of menopause
What hormonal changes occur in perimenopause and menopause (defined as 1 year of cessation of menstruation)? How does this affect the HPO axis?
Perimenopause: Reduced ability of aging follicles to secrete inhibin (produced in granulosa cells of developing follicles) lack of negative feedback from ↓inhibin ↑FSH↑ovarian follicular response maintain overall estrogen levels
Menopause: Ovarian follicles undergo accelerated loss until depletion of follicles ↓ovarian steroid hormone (estrogen, progesterone) release lack of negative feedback ↑ GnRH release↑ circulating FSH and LH
What are common symptoms of menopause? What is the pathophysiology?
Abnormal uterine bleeding– increased anovulatory cycles; With ↑unopposed estrogen levels increasing risk for developing hyperplasia/carcinoma
Vasomotor symptoms (hot flashes): occur in up to 80% of women; lasts 1-5 minutes, sudden wave of heat that spreads over the body, particularly the upper body & face; associated with sweating, palpitations, anxiety, sleep disturbance
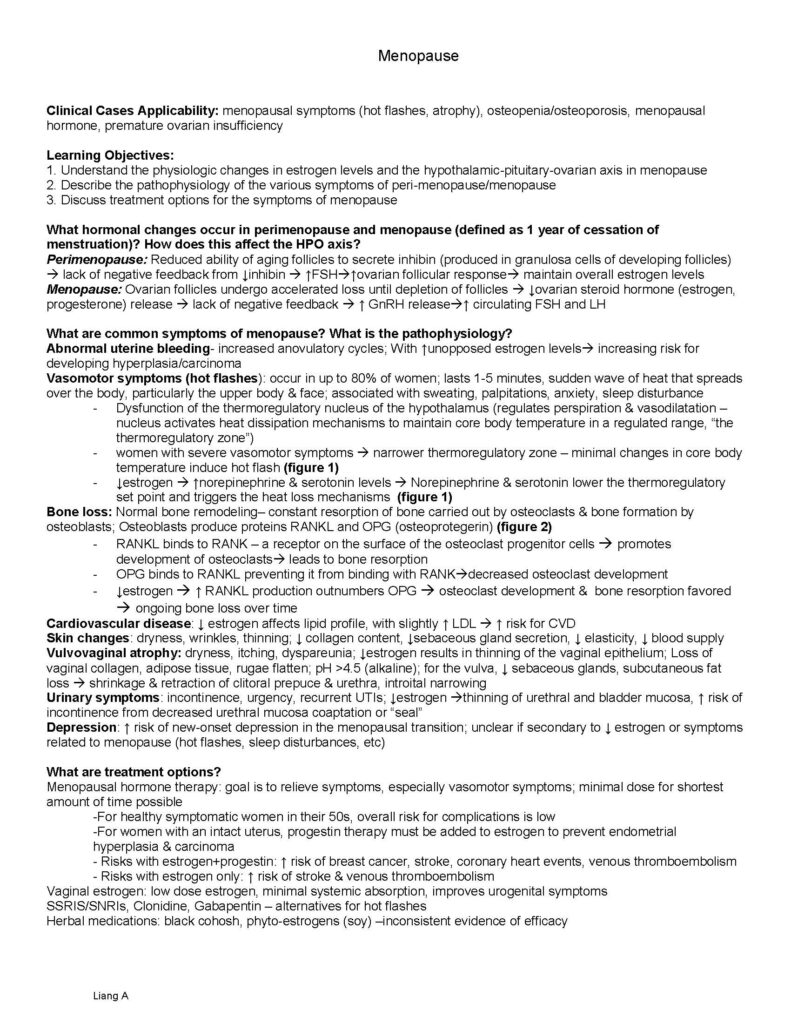
– Dysfunction of the thermoregulatory nucleus of the hypothalamus (regulates perspiration & vasodilatation –nucleus activates heat dissipation mechanisms to maintain core body temperature in a regulated range, “the thermoregulatory zone”)
– women with severe vasomotor symptoms narrower thermoregulatory zone – minimal changes in core body temperature induce hot flash (figure 1)
– ↓estrogen ↑norepinephrine & serotonin levels Norepinephrine & serotonin lower the thermoregulatory set point and triggers the heat loss mechanisms (figure 1)
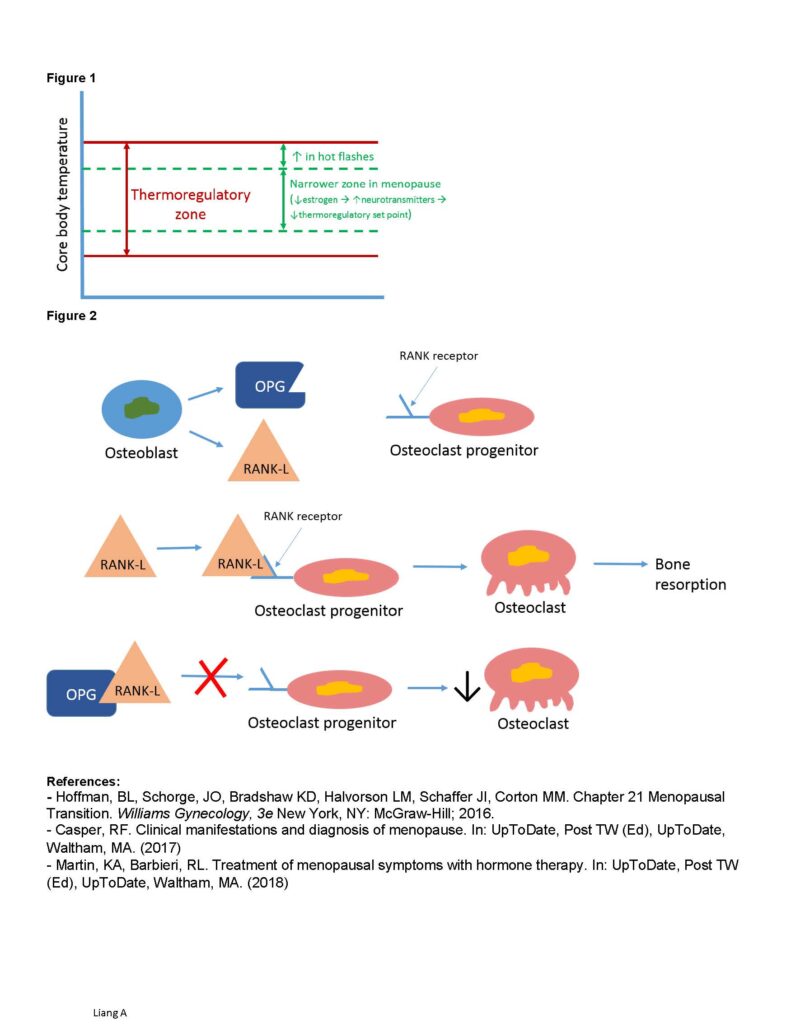
Bone loss: Normal bone remodeling– constant resorption of bone carried out by osteoclasts & bone formation by osteoblasts; Osteoblasts produce proteins RANKL and OPG (osteoprotegerin) (figure 2)
– RANKL binds to RANK – a receptor on the surface of the osteoclast progenitor cells promotes development of osteoclasts leads to bone resorption
– OPG binds to RANKL preventing it from binding with RANKdecreased osteoclast development
– ↓estrogen ↑ RANKL production outnumbers OPG osteoclast development & bone resorption favored ongoing bone loss over time
Cardiovascular disease: ↓ estrogen affects lipid profile, with slightly ↑ LDL ↑ risk for CVD
Skin changes: dryness, wrinkles, thinning; ↓ collagen content, ↓sebaceous gland secretion, ↓ elasticity, ↓ blood supply
Vulvovaginal atrophy: dryness, itching, dyspareunia; ↓estrogen results in thinning of the vaginal epithelium; Loss of vaginal collagen, adipose tissue, rugae flatten; pH >4.5 (alkaline); for the vulva, ↓ sebaceous glands, subcutaneous fat loss shrinkage & retraction of clitoral prepuce & urethra, introital narrowing
Urinary symptoms: incontinence, urgency, recurrent UTIs; ↓estrogen thinning of urethral and bladder mucosa, ↑ risk of incontinence from decreased urethral mucosa coaptation or “seal”
Depression: ↑ risk of new-onset depression in the menopausal transition; unclear if secondary to ↓ estrogen or symptoms related to menopause (hot flashes, sleep disturbances, etc)
What are treatment options?
Menopausal hormone therapy: goal is to relieve symptoms, especially vasomotor symptoms; minimal dose for shortest amount of time possible
-For healthy symptomatic women in their 50s, overall risk for complications is low
-For women with an intact uterus, progestin therapy must be added to estrogen to prevent endometrial hyperplasia & carcinoma
– Risks with estrogen+progestin: ↑ risk of breast cancer, stroke, coronary heart events, venous thromboembolism
– Risks with estrogen only: ↑ risk of stroke & venous thromboembolism
Vaginal estrogen: low dose estrogen, minimal systemic absorption, improves urogenital symptoms
SSRIS/SNRIs, Clonidine, Gabapentin – alternatives for hot flashes
Herbal medications: black cohosh, phyto-estrogens (soy) –inconsistent evidence of efficacy Liang A
Figure 1
Figure 2
References:
– Hoffman, BL, Schorge, JO, Bradshaw KD, Halvorson LM, Schaffer JI, Corton MM. Chapter 21 Menopausal Transition. Williams Gynecology, 3e New York, NY: McGraw-Hill; 2016.
– Casper, RF. Clinical manifestations and diagnosis of menopause. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2017)
– Martin, KA, Barbieri, RL. Treatment of menopausal symptoms with hormone therapy. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2018)