Mullerian Anomalies
Duration 9:34
Mullerian Anomalies
Jehnsen J, Liang A
Clinical cases applicability: Mullerian anomalies, primary amenorrhea, recurrent pregnancy loss
Learning objectives:
1) Describe the embryologic origins of the reproductive tract
2) Identify genes and hormones involved in sexual differentiation
3) Understand the mechanisms of how Mullerian anomalies form
What are the embryologic origins of the reproductive system?
Mesoderm Urogenital ridge
1) Genital ridge undifferentiated gonad ovary/testis
2) Nephrogenic cord kidneys
3) Paramesonephric (Mullerian) ducts fallopian tubes, uterus, upper vagina
4) Mesonephric (Wolffian) ducts ureters, male genital ducts, seminal vesicles
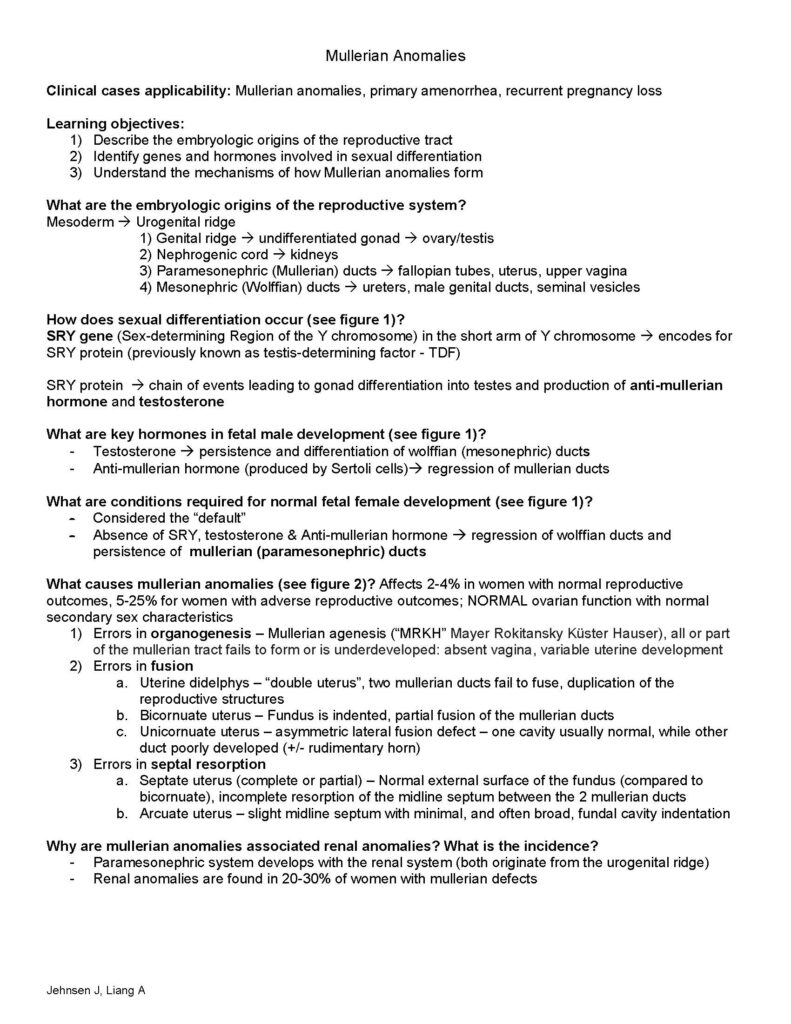
How does sexual differentiation occur (see figure 1)?
SRY gene (Sex-determining Region of the Y chromosome) in the short arm of Y chromosome encodes for SRY protein (previously known as testis-determining factor – TDF)
SRY protein chain of events leading to gonad differentiation into testes and production of anti-mullerian hormone and testosterone
What are key hormones in fetal male development (see figure 1)?
– Testosterone persistence and differentiation of wolffian (mesonephric) ducts
– Anti-mullerian hormone (produced by Sertoli cells) regression of mullerian ducts
What are conditions required for normal fetal female development (see figure 1)?
– Considered the “default”
– Absence of SRY, testosterone & Anti-mullerian hormone regression of wolffian ducts and persistence of mullerian (paramesonephric) ducts
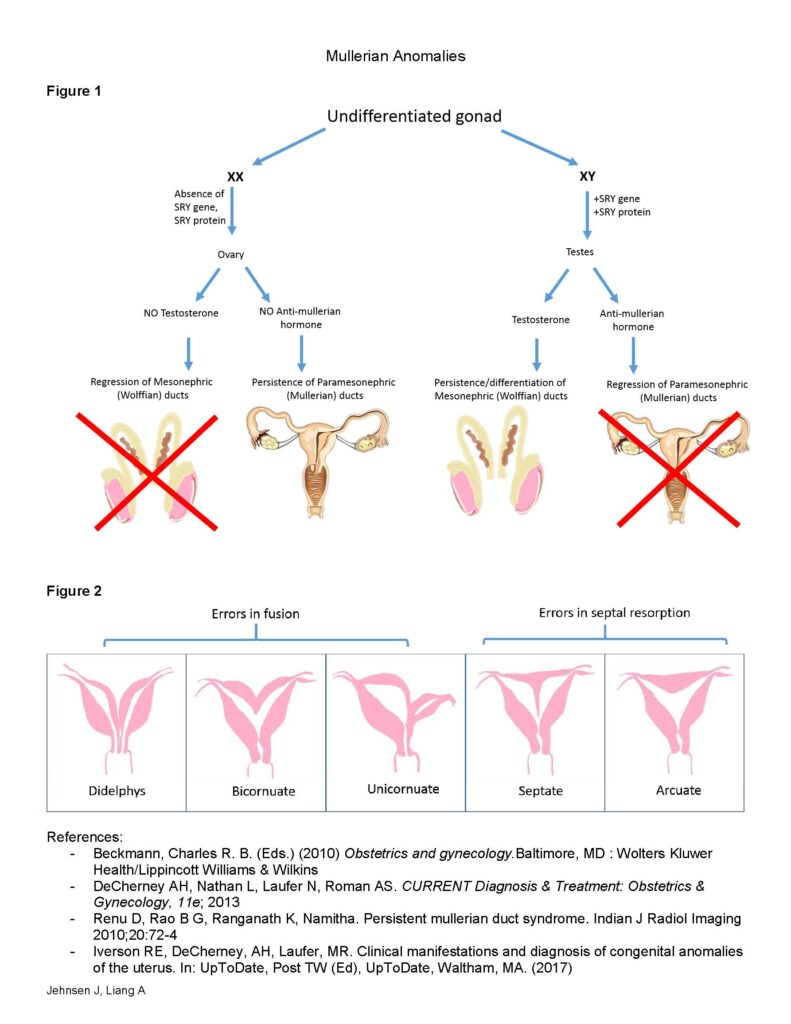
What causes mullerian anomalies (see figure 2)? Affects 2-4% in women with normal reproductive outcomes, 5-25% for women with adverse reproductive outcomes; NORMAL ovarian function with normal secondary sex characteristics
1) Errors in organogenesis – Mullerian agenesis (“MRKH” Mayer Rokitansky Küster Hauser), all or part of the mullerian tract fails to form or is underdeveloped: absent vagina, variable uterine development
2) Errors in fusion
a. Uterine didelphys – “double uterus”, two mullerian ducts fail to fuse, duplication of the reproductive structures
b. Bicornuate uterus – Fundus is indented, partial fusion of the mullerian ducts
c. Unicornuate uterus – asymmetric lateral fusion defect – one cavity usually normal, while other duct poorly developed (+/- rudimentary horn)
3) Errors in septal resorption
a. Septate uterus (complete or partial) – Normal external surface of the fundus (compared to bicornuate), incomplete resorption of the midline septum between the 2 mullerian ducts
b. Arcuate uterus – slight midline septum with minimal, and often broad, fundal cavity indentation
Why are mullerian anomalies associated renal anomalies? What is the incidence?
– Paramesonephric system develops with the renal system (both originate from the urogenital ridge)
– Renal anomalies are found in 20-30% of women with mullerian defects
Mullerian Anomalies
Jehnsen J, Liang A
Figure 1
Figure 2
References:
– Beckmann, Charles R. B. (Eds.) (2010) Obstetrics and gynecology.Baltimore, MD : Wolters Kluwer Health/Lippincott Williams & Wilkins
– DeCherney AH, Nathan L, Laufer N, Roman AS. CURRENT Diagnosis & Treatment: Obstetrics & Gynecology, 11e; 2013
– Renu D, Rao B G, Ranganath K, Namitha. Persistent mullerian duct syndrome. Indian J Radiol Imaging 2010;20:72-4
– Iverson RE, DeCherney, AH, Laufer, MR. Clinical manifestations and diagnosis of congenital anomalies of the uterus. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2017)