Physiology of the Menstrual Cycle
Duration 11:16
Physiology of the Menstrual Cycle
Clinical Cases Applicability:
Menarche, Menopause, Oligomenorrhea/Amenorrhea, Contraception
Learning Objectives:
1) Summarize how the hypothalamic-pituitary-ovarian (HPO) axis regulates ovarian function and the menstrual cycle
2) Explain how the HPO defines the phases of the menstrual cycle
3) Differentiate between how the HPO axis interacts to define the stages of the reproductive cycle—puberty, menstruation,
menopause
Clinical Presentation:
Oligomenorrhea and Infertility, Puberty onset, Menopausal symptoms
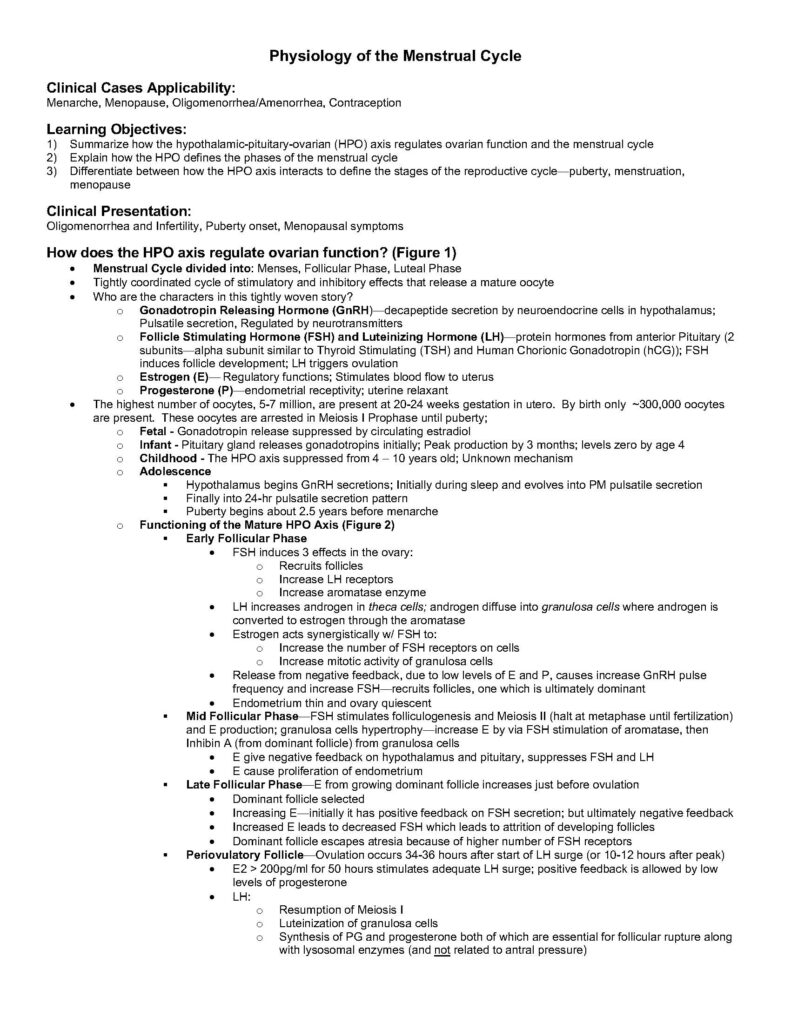
How does the HPO axis regulate ovarian function? (Figure 1)
• Menstrual Cycle divided into: Menses, Follicular Phase, Luteal Phase
• Tightly coordinated cycle of stimulatory and inhibitory effects that release a mature oocyte
• Who are the characters in this tightly woven story?
o Gonadotropin Releasing Hormone (GnRH)—decapeptide secretion by neuroendocrine cells in hypothalamus;
Pulsatile secretion, Regulated by neurotransmitters
o Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH)—protein hormones from anterior Pituitary (2
subunits—alpha subunit similar to Thyroid Stimulating (TSH) and Human Chorionic Gonadotropin (hCG)); FSH
induces follicle development; LH triggers ovulation
o Estrogen (E)— Regulatory functions; Stimulates blood flow to uterus
o Progesterone (P)—endometrial receptivity; uterine relaxant
• The highest number of oocytes, 5-7 million, are present at 20-24 weeks gestation in utero. By birth only ~300,000 oocytes
are present. These oocytes are arrested in Meiosis I Prophase until puberty;
o Fetal – Gonadotropin release suppressed by circulating estradiol
o Infant – Pituitary gland releases gonadotropins initially; Peak production by 3 months; levels zero by age 4
o Childhood – The HPO axis suppressed from 4 – 10 years old; Unknown mechanism
o Adolescence
§ Hypothalamus begins GnRH secretions; Initially during sleep and evolves into PM pulsatile secretion
§ Finally into 24-hr pulsatile secretion pattern
§ Puberty begins about 2.5 years before menarche
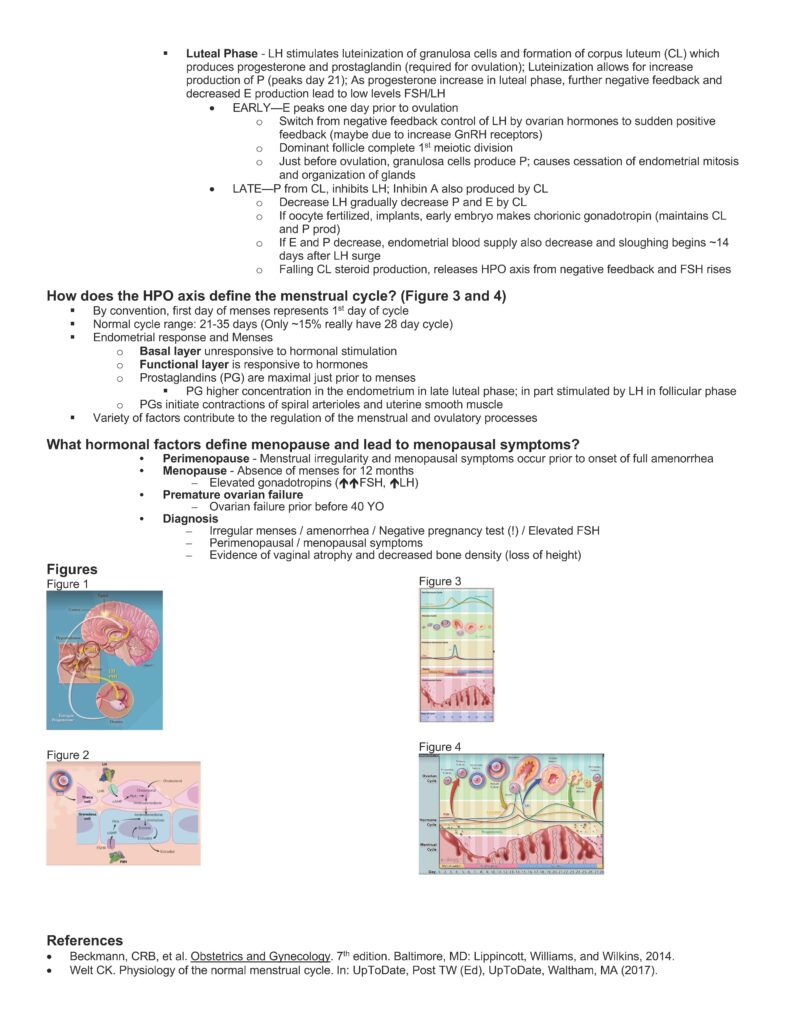
o Functioning of the Mature HPO Axis (Figure 2)
§ Early Follicular Phase
• FSH induces 3 effects in the ovary:
o Recruits follicles
o Increase LH receptors
o Increase aromatase enzyme
• LH increases androgen in theca cells; androgen diffuse into granulosa cells where androgen is
converted to estrogen through the aromatase
• Estrogen acts synergistically w/ FSH to:
o Increase the number of FSH receptors on cells
o Increase mitotic activity of granulosa cells
• Release from negative feedback, due to low levels of E and P, causes increase GnRH pulse
frequency and increase FSH—recruits follicles, one which is ultimately dominant
• Endometrium thin and ovary quiescent
§ Mid Follicular Phase—FSH stimulates folliculogenesis and Meiosis II (halt at metaphase until fertilization)
and E production; granulosa cells hypertrophy—increase E by via FSH stimulation of aromatase, then
Inhibin A (from dominant follicle) from granulosa cells
• E give negative feedback on hypothalamus and pituitary, suppresses FSH and LH
• E cause proliferation of endometrium
§ Late Follicular Phase—E from growing dominant follicle increases just before ovulation
• Dominant follicle selected
• Increasing E—initially it has positive feedback on FSH secretion; but ultimately negative feedback
• Increased E leads to decreased FSH which leads to attrition of developing follicles
• Dominant follicle escapes atresia because of higher number of FSH receptors
§ Periovulatory Follicle—Ovulation occurs 34-36 hours after start of LH surge (or 10-12 hours after peak)
• E2 > 200pg/ml for 50 hours stimulates adequate LH surge; positive feedback is allowed by low
levels of progesterone
• LH:
o Resumption of Meiosis I
o Luteinization of granulosa cells
o Synthesis of PG and progesterone both of which are essential for follicular rupture along
with lysosomal enzymes (and not related to antral pressure)
§ Luteal Phase – LH stimulates luteinization of granulosa cells and formation of corpus luteum (CL) which
produces progesterone and prostaglandin (required for ovulation); Luteinization allows for increase
production of P (peaks day 21); As progesterone increase in luteal phase, further negative feedback and
decreased E production lead to low levels FSH/LH
• EARLY—E peaks one day prior to ovulation
o Switch from negative feedback control of LH by ovarian hormones to sudden positive
feedback (maybe due to increase GnRH receptors)
o Dominant follicle complete 1st meiotic division
o Just before ovulation, granulosa cells produce P; causes cessation of endometrial mitosis
and organization of glands
• LATE—P from CL, inhibits LH; Inhibin A also produced by CL
o Decrease LH gradually decrease P and E by CL
o If oocyte fertilized, implants, early embryo makes chorionic gonadotropin (maintains CL
and P prod)
o If E and P decrease, endometrial blood supply also decrease and sloughing begins ~14
days after LH surge
o Falling CL steroid production, releases HPO axis from negative feedback and FSH rises
How does the HPO axis define the menstrual cycle? (Figure 3 and 4)
§ By convention, first day of menses represents 1st day of cycle
§ Normal cycle range: 21-35 days (Only ~15% really have 28 day cycle)
§ Endometrial response and Menses
o Basal layer unresponsive to hormonal stimulation
o Functional layer is responsive to hormones
o Prostaglandins (PG) are maximal just prior to menses
§ PG higher concentration in the endometrium in late luteal phase; in part stimulated by LH in follicular phase
o PGs initiate contractions of spiral arterioles and uterine smooth muscle
§ Variety of factors contribute to the regulation of the menstrual and ovulatory processes
What hormonal factors define menopause and lead to menopausal symptoms?
• Perimenopause – Menstrual irregularity and menopausal symptoms occur prior to onset of full amenorrhea
• Menopause – Absence of menses for 12 months
– Elevated gonadotropins (ééFSH, éLH)
• Premature ovarian failure
– Ovarian failure prior before 40 YO
• Diagnosis
– Irregular menses / amenorrhea / Negative pregnancy test (!) / Elevated FSH
– Perimenopausal / menopausal symptoms
– Evidence of vaginal atrophy and decreased bone density (loss of height)
Figures
Figure 1
Figure 2
Figure 3
Figure 4
References
• Beckmann, CRB, et al. Obstetrics and Gynecology. 7th edition. Baltimore, MD: Lippincott, Williams, and Wilkins, 2014.
• Welt CK. Physiology of the normal menstrual cycle. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA (2017).