Endometrial Hyperplasia and Endometrial Intraepithelial Neoplasia
Duration 9:24
Benign Endometrial Hyperplasia and Endometrial Intraepithelial Neoplasia (EIN)
Liang A
Clinical Cases Applicability: Abnormal uterine bleeding, ovulatory dysfunction, post-menopausal bleeding, endometrial cancer
Learning Objectives:
1) Describe the histology of the endometrium, and changes associated with hormonal fluctuation
2) Describe the histopathology of endometrial hyperplasia and EIN
3) Understand the role of progestins in treating hyperplasia
NORMAL ENDOMETRIUM
What is the structure of the endometrium?
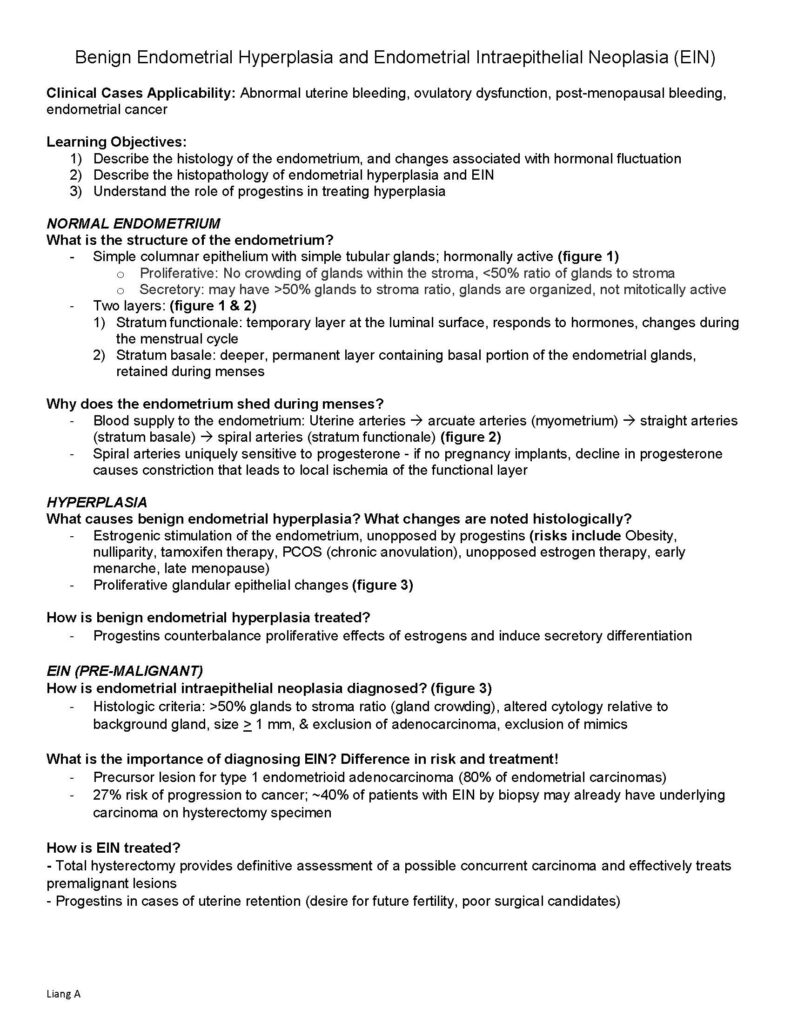
– Simple columnar epithelium with simple tubular glands; hormonally active (figure 1)
o Proliferative: No crowding of glands within the stroma, <50% ratio of glands to stroma
o Secretory: may have >50% glands to stroma ratio, glands are organized, not mitotically active
– Two layers: (figure 1 & 2)
1) Stratum functionale: temporary layer at the luminal surface, responds to hormones, changes during the menstrual cycle
2) Stratum basale: deeper, permanent layer containing basal portion of the endometrial glands, retained during menses
Why does the endometrium shed during menses?
– Blood supply to the endometrium: Uterine arteries arcuate arteries (myometrium) straight arteries (stratum basale) spiral arteries (stratum functionale) (figure 2)
– Spiral arteries uniquely sensitive to progesterone – if no pregnancy implants, decline in progesterone causes constriction that leads to local ischemia of the functional layer
HYPERPLASIA
What causes benign endometrial hyperplasia? What changes are noted histologically?
– Estrogenic stimulation of the endometrium, unopposed by progestins (risks include Obesity, nulliparity, tamoxifen therapy, PCOS (chronic anovulation), unopposed estrogen therapy, early menarche, late menopause)
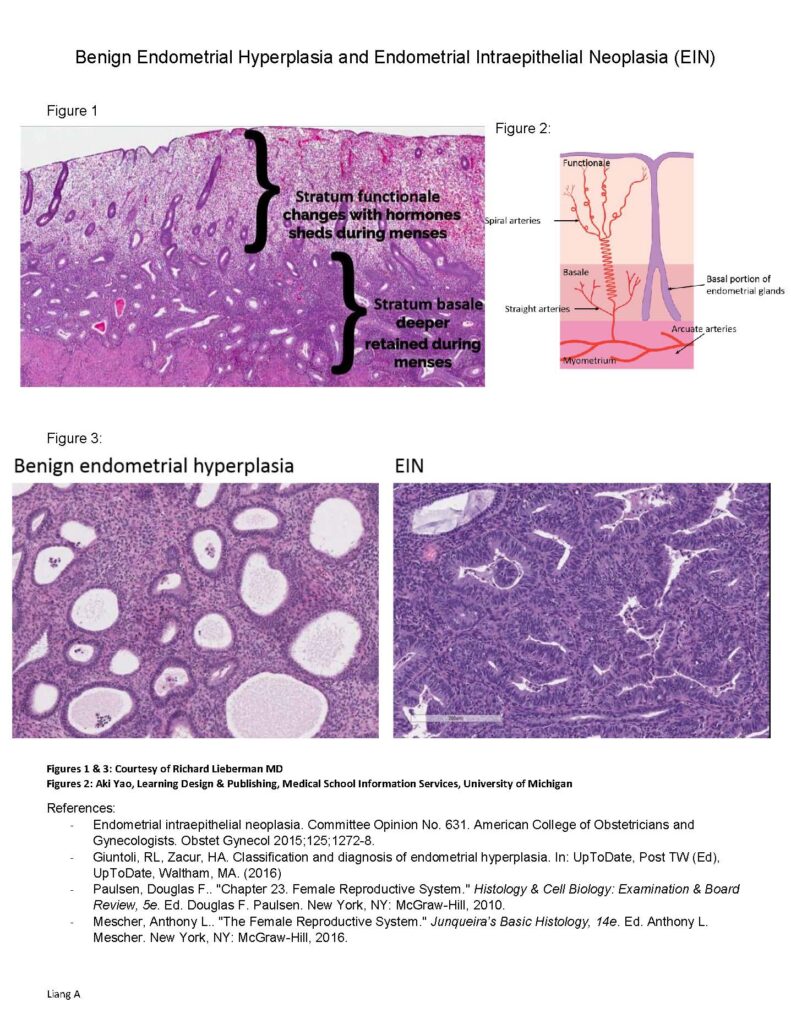
– Proliferative glandular epithelial changes (figure 3)
How is benign endometrial hyperplasia treated?
– Progestins counterbalance proliferative effects of estrogens and induce secretory differentiation
EIN (PRE-MALIGNANT)
How is endometrial intraepithelial neoplasia diagnosed? (figure 3)
– Histologic criteria: >50% glands to stroma ratio (gland crowding), altered cytology relative to background gland, size > 1 mm, & exclusion of adenocarcinoma, exclusion of mimics
What is the importance of diagnosing EIN? Difference in risk and treatment!
– Precursor lesion for type 1 endometrioid adenocarcinoma (80% of endometrial carcinomas)
– 27% risk of progression to cancer; ~40% of patients with EIN by biopsy may already have underlying carcinoma on hysterectomy specimen
How is EIN treated?
– Total hysterectomy provides definitive assessment of a possible concurrent carcinoma and effectively treats premalignant lesions
– Progestins in cases of uterine retention (desire for future fertility, poor surgical candidates) Benign Endometrial Hyperplasia and Endometrial Intraepithelial Neoplasia (EIN)
Liang A
Figure 1
Figure 2:
Figure 3:
Figures 1 & 3: Courtesy of Richard Lieberman MD
Figures 2: Aki Yao, Learning Design & Publishing, Medical School Information Services, University of Michigan
References:
– Endometrial intraepithelial neoplasia. Committee Opinion No. 631. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;125;1272-8.
– Giuntoli, RL, Zacur, HA. Classification and diagnosis of endometrial hyperplasia. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (2016)
– Paulsen, Douglas F.. “Chapter 23. Female Reproductive System.” Histology & Cell Biology: Examination & Board Review, 5e. Ed. Douglas F. Paulsen. New York, NY: McGraw-Hill, 2010.
– Mescher, Anthony L.. “The Female Reproductive System.” Junqueira’s Basic Histology, 14e. Ed. Anthony L. Mescher. New York, NY: McGraw-Hill, 2016.